The use of system biology approach using information from the genome, proteome, metabolome, transcriptome is being increasing used to predict the strategies for treating individuals.
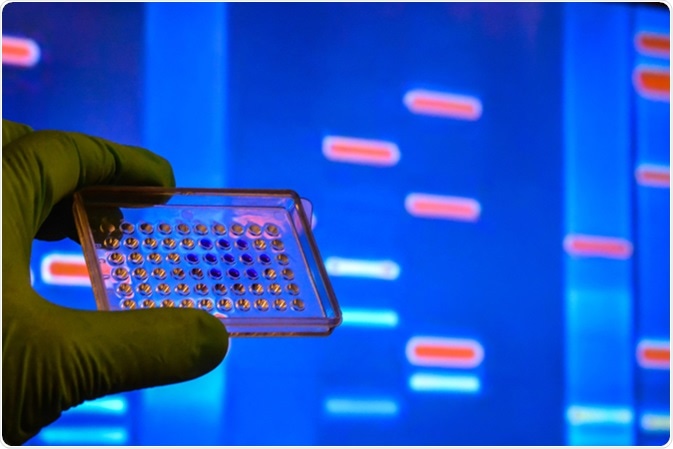
Image Credit: Sergei Drozd / Shutterstock
What is Personalized or Precision Medicine?
There is a lot of variability in the genetic make-up of individuals. The concept of personalized medicine recognizes this and predicts the treatment strategy based on the genome-wide data collected at the level of an individual. It uses biomarkers, such as genes, transcripts, proteins, and metabolites to understand the biology of a patient.
This is different from the traditional methods which use a single solution for an entire population who may differ widely in terms of their genome. Thus, personalized medicine predicts the normal and pathogenic state of an individual based on the genes and their interaction with specific environments.
Omics in Translational and Clinical Medicine
Several omic technologies are being used to derive and predict solutions for diseased states.
High throughput sequencing technology
Next-generation sequencing (NGS) is being used to study genome, epigenome, and transcriptome. NGS strategies are being used to develop diagnostic solutions based on sequencing of either key protein coding regions, the entire genome (whole genome sequencing or WGS), or exons (whole exome sequencing or WES). These strategies can be used to find the variations present in the native or disease states of an individual.
Mass spectrometry based omics
Mass spectrometry (MS) is used to weigh and separate molecules based on their mass to charge ratios. MS instruments can be used in combination with liquid or gas chromatography, capillary electrophoresis, and ion mobility to increase their sensitivity and specificity. As this technique is highly sensitive, MS is preferred to derive information about personalized differences in the metabolome and proteome.
Phenomics
Phenomics is a branch which measures the physical and chemical outcome of interactions between genes and environment using quantitative measurements. This method can measure how an individual’s interaction with the environment can change our genes. To measure this, deep phenotyping (DP) and phenomics analysis (PA) are employed. DP involves clinical assessment, lab analysis and imaging, while PA evaluates the patterns between individuals with related phenotypes. It uses clinical data, visualization, and data integration to provide inferences.
(Video 1 of 8) Introduction to Omics: 360 Degree View of You
Limitations of Omics Analysis
Presence of experimental and analytical noise
Two parameters are critical for research: reproducibility and repeatability. However, high throughput data can have large batch effects or technical sources of variation during handling large number of samples. This creates an important confounder in such studies. Different manufacturers provide different platforms for same type of omics. There are multiple versions of microarray and sequencing platforms for genomics, epigenomics and transcriptome association studies. Similarly, different MS platforms may have different sensitivities and specificities. This creates differences in resolution and thus variation.
Biological variation
Biological variation may also generate discrepancies in data and its inference. Although genetic profiles will be similar across tissues and cell types, all the other profiles, such transcriptome, metabolome and phenome are highly dependent on the sample. Different factors, such as diet, circadian rhythm, and drugs may induce differences. Data can change depending on the location and physiological state of the tissue. Thus, appropriate statistical measures have to be employed to negate the cell-to-cell variabilities.
Further Reading
Last Updated: Feb 27, 2019