In a recent review published in the journal BMC Global and Public Health, researchers explored the current evidence on nutritionally acquired immunodeficiency syndrome (N-AIDS). They discussed why N-AIDS needs to be recognized as a crucial determinant and comorbidity among tuberculosis (TB) patients across the globe. They have emphasized the importance of addressing nutrition with a priority equivalent to human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) to mitigate the TB pandemic and improve overall outcomes.
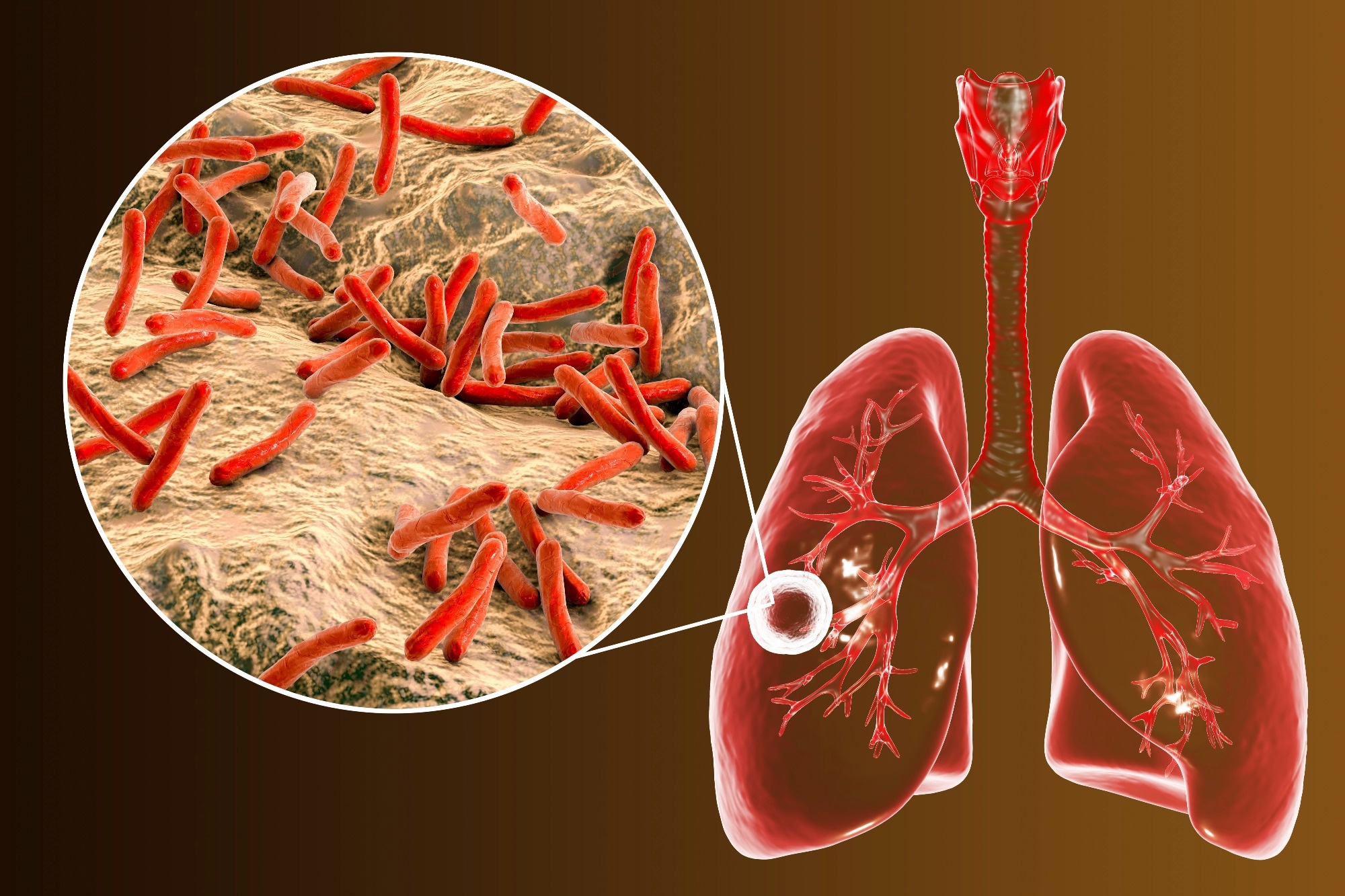 Perspective: Nutritionally acquired immunodeficiency must be addressed with the same urgency as HIV to end tuberculosis. Image Credit: Kateryna Kon / Shutterstock
Perspective: Nutritionally acquired immunodeficiency must be addressed with the same urgency as HIV to end tuberculosis. Image Credit: Kateryna Kon / Shutterstock
Background
Research in the past few decades has helped establish HIV as a determinant and comorbidity of TB, leading to integrated screening and care protocols. However, malnutrition, or N-AIDS, emerges as the primary cause of secondary immunodeficiency. Malnourished individuals, akin to those with HIV, face increased infection risks, and the association between malnutrition and TB has been established for a century. The current review emphasizes the recognition of malnutrition as a significant determining factor and comorbidity of TB to accelerate detection, treatment, and prevention efforts aimed at addressing the TB pandemic.
Detection of TB
Early detection and treatment of TB are essential for eliminating the disease, especially considering that more than four million TB cases go undiagnosed globally. Individuals with active TB remain contagious for months before diagnosis, underscoring the need for earlier intervention. Weight loss is a subtle yet significant symptom, with over 50% of TB patients in high-burden countries being malnourished at diagnosis. The World Health Organization (WHO) recommends systematic TB screening in populations where prevalence exceeds 0.5%. Studies in Myanmar and India reveal higher TB prevalence among malnourished individuals, justifying systematic screening in this vulnerable group. However, current screening primarily focuses on clinical TB, overlooking subclinical disease and hidden nutritional deficiencies. Malnutrition's impact on test performance, especially in triage tests, necessitates optimization for accurate diagnosis in malnourished populations. Concurrent screening for malnutrition and TB involving better indicators than body mass index (BMI) is crucial, calling for improved detection strategies targeting the at-risk population.
Treatment of TB
Despite the proven impact of weight gain on TB therapy outcomes, malnourished individuals continue to experience worse health outcomes post-treatment. Severely malnourished individuals face a twofold higher risk of unfavorable treatment outcomes, including death. Malnutrition impairs the immune response to TB, leading to more severe disease manifestations. Pharmacotherapy effectiveness is compromised in malnourished individuals, impacting drug exposure and toxicity risks. Lack of access to food during TB therapy can result in treatment discontinuation. Nutritional status assessment should be a standard part of TB therapy, comparable to HIV testing. The neglect of malnutrition in TB management is evident in the absence of tailored nutritional interventions and tools for assessing nutritional status. Nutritional support for individuals with TB has demonstrated improved treatment success rates, thereby aiding adherence and reducing financial strain. Addressing malnutrition in TB management is important, not only for disease outcomes but also for individuals' overall well-being and potential.
Prevention of TB
Natural experiments during World Wars I and II highlighted the inverse relationship between malnutrition and TB rates. Prospective analyses, such as NHANES I, reveal a 12-fold increase in TB among underweight individuals. While studies often use BMI, compelling data also link micronutrients to TB risk. The RATIONS study in India demonstrated a 40% reduction in incident TB with nutritional support. Health-economic models project significant reductions in TB incidence and mortality with population-scale malnutrition reduction, emphasizing the cost-effectiveness of such interventions. Recognizing food as an adjunct to TB vaccines, research should explore the immunology of malnutrition to enhance vaccine efficacy, ensuring effectiveness in malnourished populations.
Conclusion and Future Perspectives
Recognition of malnutrition as a critical TB comorbidity is essential, demanding integrated nutritional screening in TB programs akin to HIV testing. Adhering to the WHO guidelines and reporting malnutrition rates among persons with TB (PWTB) in global TB reports may help address the issue. TB programs should provide nutritional counseling alongside in-kind or cash support, leveraging existing infrastructure. Coordination across sectors and collaboration with international bodies are imperative for a holistic approach. Researchers should include nutritional screening in studies, addressing variations in nutritional needs across demographics. Increased funding for operational research on nutrition and TB is the need of the hour.
For decades, data have consistently linked malnutrition to the TB pandemic, yet N-AIDS lacks prioritized assessment and care, unlike HIV. Acknowledging malnutrition as a dominant TB driver is key to the End-TB strategy's success. With simple interventions, significant reductions in TB incidence and mortality are achievable through nutrition investments. The global health community, having tackled one form of AIDS, can similarly address N-AIDS in detecting, treating, and preventing TB.