By Dr Stephen Tuft, MD FRCOphth
What is the cornea?
The avascular cornea is the curved and transparent window at the front of the eye. It provides the majority of the focus for light entering the eye to produce an image on the retina. Because the cornea is so important for forming an image, any change in corneal shape (astigmatism) or opacity has a major impact on the quality of vision. Intentionally changing the radius of curvature of the cornea is the basis of laser surgery to correct refractive error.

Laser eye surgery © goir / Shutterstock.com
Contact lenses worn on the surface of the cornea are an increasingly popular alternative to glasses, but contact lens associated corneal infection has become a significant public health problem in developed countries.
The cornea consists of a number of distinct layers (Figure). The surface epithelium supports the tear film and is maintained by a population of stem cells located in the basal layer of cells at the limbus – the junction between the clear cornea and the opaque sclera.
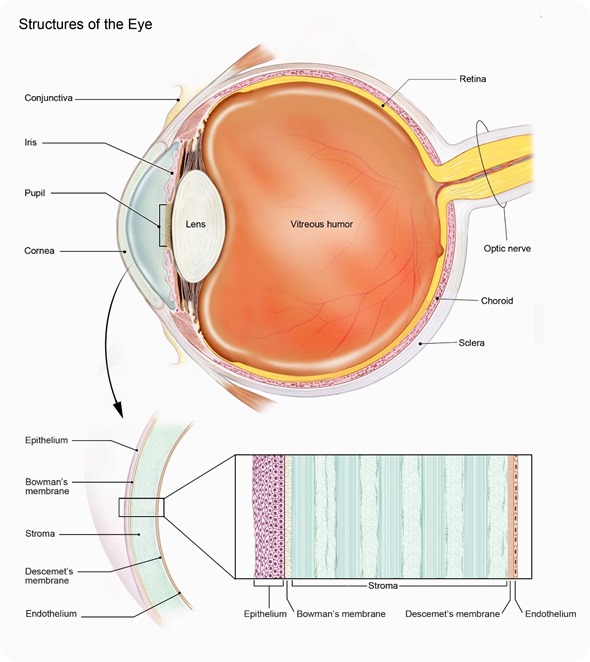
Beneath the epithelium is the fibrous stroma that maintains its transparency through its relative state of dehydration, regular collagen fibre spacing, and ordered collagen and proteoglycan distribution. The endothelial monolayer on the internal surface of the cornea actively pumps water from the cornea. The endothelium has minimal regenerative capacity and damage can result in permanent corneal swelling and opacity.
Corneal disease is a major cause for visual loss worldwide. It has been estimated that in 2002 corneal disease accounted for approximately 5% of world blindness (1.8m individuals), with four times that number having significant visual impairment.1
Corneal disease is also reported to be the reason for 4.1% of blind registrations in the UK. There are wide regional differences in the causes for corneal blindness. In developing and rural communities trauma or infection are the principal causes.
In contrast, in developed countries, genetically determinant diseases are more important. Between 2015 and 2016 there were 3466 corneal transplants reported to the UK transplant registry, with keratoconus, Fuchs endothelial corneal dystrophy, and other dystrophies accounted for the majority (50.9%) of these transplants. Infection, keratitis and corneal neovascularisation are also important causes for sight loss.
Although corneal transplantation is often effective in terms of graft survival, the quality of vision may not be restored and better alternatives are required.
The recent publication of a review of new and emerging health technologies for corneal disorders has highlighted the primary areas of research interest. Specific emphasis was found for refractive error (astigmatism), endothelial disease, infection, and epithelial stem cell deficiency.2 The following areas of research interest were noted.
Regenerative medicine
A chronic epithelial defect, corneal ulceration, and opacity may result from aberrant wound healing and stromal regeneration. Corneal tissue engineering uses synthetic biocompatible substitutes or substrates as a matrix to support tissue repair with eventual integration.
Approaches include a regenerative glue for patching corneal perforation, recombinant human nerve growth factor to promote healing of the anaesthetic cornea, and the topical application of synthetic stromal matrix proteoglycans (e.g. decoran, heparan) to act as a scaffold to promote wound repair.
Infection
Fortunately, microbial resistance is not yet a major problem in the UK. However, corneal infection with protozoa (acanthamoeba) and filamentary fungi associated with contact lens wear are becoming more common.
These infections are difficult to eradicate from the cornea, options are limited, and better treatments are required. A randomised control of topical polyhexanide (PHMB) will begin in 2017.
Improvement of contact lens design and storage to reduce risk of contamination and infection is ongoing. The rapid molecular diagnosis of these infectious pathogens with PCR may help guide early therapy and aid targeted treatment according to susceptibility to treatment and virulence.
Transplantation
Corneal transplantation is an option for corneal opacity, perforation, severe astigmatism, and epithelial surface or endothelial cell failure. The emergence of partial thickness (lamellar) surgical techniques and an associated lowering of the threshold for intervention has increased demand for tissue, with a 75% increase in procedures since 2000.
Pioneering work on cultured endothelial cell transplantation has seen a step-change in our thinking on treatments for endothelial disease. This is the subject of a clinical trial, and cell transplantation is likely to become available within a 10-year timeframe. This would greatly expand the availability of tissue for transplantation.
Limbal epithelial transplantation has become a routine procedure for ocular surface epithelial failure, but the major disease group for ocular surface reconstruction are patients with bilateral disease, in which auto-transplantation from the unaffected eye is not an option.
Development of auto-transplants from other epithelial sources (e.g. mouth, bladder) such that lifelong immunosuppression would not be required would be a major advance. The identification of a role for corneal stromal mesenchymal stem cells to modify scar formation has opened exciting new therapeutic options.
Severe dry eye disease is associated with a change in phenotype of the ocular surface cells and is a major cause for failure of many interventions, e.g. transplantation and some designs of keratoprosthesis. Treatment options for these patients remain severely limited.
Artificial cornea (keratoprosthesis)
These are currently the option of choice if a tissue transplant is unlikely to work due to severe dry eye disease, inflammation, or a high risk of allograft rejection from corneal vascularisation. As they are inert polymers systemic immunosuppression is not required.
Designs continue to improve but extrusion or resorption of the supporting tissue remains a problem and improved biocompatibility is required.
Gene based therapies
The most recent audit of UK Transplant reported that 50.7% of grafts performed 2015 to 2016 were for inherited corneal disease. Identification of the causative genes will open doors to earlier diagnosis and intervention, as well as novel treatments.
The clinical introduction of gene silencing technologies to suppress the formation of aberrant cell products in a likely development within the next decade. Gene-based approaches to inhibit corneal vascularisation – a major risk for transplant rejection - and to alter the immunogenicity of donor corneal tissue may expand the options for individual with disease that currently precludes the use of a transplant.
As the genetic basis for more corneal diseases are understood new targeted treatments will become available, e.g. the introduction of topical cysteamine drops for corneal cystinosis.
Corneal collagen cross linkage
Keratoconus affects in excess of 55,000 individuals in the UK. It can cause severe visual loss in young adults and is the second commonest reason for corneal transplantation in the UK. Photochemical cross linking of the cornea can prevent further progression of keratoconus in approximately 95% of individuals, and the emphasis is now on methods to identify and treat individuals at risk of sight loss at a stage where they still have good unaided or spectacle corrected vision.
There will probably be a shift to pre-emptive intervention at first diagnosis as safer treatment option become available. A downstream effect should be a reduced demand for corneal tissue for transplantation, and this effect that has already been reported from Norway with potentially a drop in 50% of transplants for keratoconus.
It is likely that there will be a drive towards screening for keratoconus in at-risk populations (i.e. in schools) hopefully aided by research to identify the causative genes. Better connectivity between community optometrists and hospital based clinicians, possible with computerised algorithms to filter data, would help with this.
Conclusion
Research into the mechanisms of blinding corneal disease continues to accelerate and exciting alternatives to surgery are appearing. However, validation requires clinical trials that can be difficult to recruit and expensive to run. Although there is often an extended interval to clinical implementation of novel techniques there is a high expectation that there will be real benefits for patients.
References
1. Resnikoff S, Pascolini D, Etya'ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82(11): 844-51.
2. Horizon Scanning Research & Intelligence Centre. New and emerging health technologies for corneal disorders. University of Birmingham. 2016 (accessed 27th October 2016). https://www.nihr.ac.uk/
Acknowledgements
 Fight for sight - Someone in the world goes blind every five seconds.
Fight for sight - Someone in the world goes blind every five seconds.
Our mission is to stop sight loss in its tracks. By funding pioneering eye research, we’re creating a future everyone can see.
Further Reading
About Stephen Tuft
 Consultant Ophthalmologist
Consultant Ophthalmologist
Moorfields Eye Hospital NHS Foundation Trust
Trained as an ophthalmologist in New Zealand with further training in Adelaide, Australia. He began research at the Institute of Ophthalmology in London.
He returned to clinical work as a lecturer in the Contact Lens Service at Moorfields Eye Hospital, where he developed an interest in keratoconus, inherited eye disease and infection.
He has published numerous papers on these topics and he is currently leading a large collaborative research program to try to identify the genetic changes that cause keratoconus and treatments for Fuchs corneal dystrophy. He hopes that this work will eventually lead to better ways to screen and treat these conditions.
Disclaimer: This article has not been subjected to peer review and is presented as the personal views of a qualified expert in the subject in accordance with the general terms and condition of use of the News-Medical.Net website.