By Jeyashree Sundaram, MBA
Barrett’s esophagus (BE) is a condition where the tissues present in the esophagus undergo transformation and become similar to those found in the intestinal lining. It is present mostly in people who have gastroesophageal reflux disease (GERD), especially if it has been present for a very long period. This in turn is related to an increased risk for developing esophageal cancer.
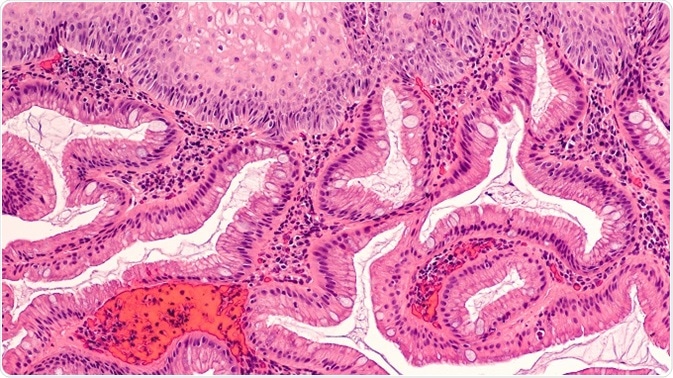
Endoscopic biopsy photomicrograph of intestinal (Barrett's) metaplasia of the esophagus. Credit: David Litman/Shutterstock.com
Risk of transformation of cells
Barrett’s esophagus does not proceed to cancer in all patients; however, it is estimated that around 10–15% of cases of BE may progress to esophageal cancer. There are two kinds of cell transformations that are associated with either squamous cell or adenocarcinoma of the esophagus.
- Squamous cell cancer of the esophagus is more common in people who drink excessively and/or smoke cigarettes. When there is a prolonged abnormal backward flow of stomach acid into the lower esophagus, it can affect the inner lining of the esophagus. Squamous cell metaplasia is caused by this process; here, the cells that line the esophagus are replaced by gland cells. These gland cells resemble the normal lining cells of the stomach and the small intestine. This, however, is not a frequently occurring cell transformation in Barrett’s esophagus.
- Adenocarcinoma of the esophagus occurs in people who have GERD. Patients who have a long history of acid reflux may develop Barrett’s esophagus. Most patients with this condition may have symptoms of heartburn, while a few do not exhibit any symptoms at all. The frequency of this type of cancer has rapidly increased over the years. Most adenocarcinomas of the esophagus start in Barrett’s tissue.
Barrett's Esophagus: The Doorstep to Throat Cancer
Risk factors
Dysplasia
Dysplasia is a condition in which cells show precancerous changes, and it can occur within Barrett’s tissue. The development of dysplasia maybe the only risk factor for cancer in BE. Dysplasia is generally defined as the stage preceding the development of frank cancer. This condition can be diagnosed by endoscopic biopsy in Barrett’s esophagus.
If dysplasia is identified by examining a biopsy under the microscope, healthcare providers often advise performing an endoscopy in order to destroy the whole of the metaplastic tissue. Though the risk of dysplasia is low, it is important to have regular checkups for dysplasia, so that it can be treated and prevented from developing into esophageal cancer.
Depending upon the level of risk possessed by the dysplasia, it can be classified into different grades: negative to dysplasia, low grade dysplasia, and high grade dysplasia.
- Without Dysplasia/ negative to dysplasia: Barrett’s esophagus without dysplasia or negative to dysplasia means that no precancerous changes were identified in the cells visualized on microscopy of the biopsy tissue. If the area of dysplasia is very small or negligible, it may be missed when the biopsy is taken. Therefore, a higher number of biopsies may be taken, or more frequent endoscopies may be performed, every 3–5 years regularly. This may help to identify and destroy the abnormal changes in the Barrett’s tissue. The risk of cancer for non-dysplastic Barrett’s esophagus is very low.
- Low grade dysplasia (LGD): In this type, the cell changes are present but minimal. Out of 100 patients with BE and low-grade dysplasia, 20 are at risk of developing cancer of the esophagus within 5 years.
- High grade dysplasia (HGD): In this type, there are abnormal changes in the cells. This is mainly linked to a higher risk of esophageal carcinoma. In 30-60% of cases, it may progress to cancer if not treated properly. HGD is a more advanced pre-cancerous condition of the esophagus than low grade dysplasia.
Both high as well as low grade dysplasia does not have the capability to spread to other parts of the body.
Risk factors for HGD
Some of the risk factors associated with the development of high grade dysplasia are:
- Segment: A recent study from Berlin has determined that segment length is associated with an increased risk of high grade dysplasia. That is, patients with long segment Barrett’s esophagus (LSBE) are at an increased risk of progression to high grade dysplasia than people with short segment Barrett’s esophagus (SSBE).
- Mucosal abnormalities: In Barrett’s esophagus, some types of mucosal changes are related to an increased risk of high grade dysplasia. Erosive and ulcerative esophagitis are associated with increased risk of progression to esophageal adenocarcinoma or high grade dysplasia.
The greatest risk for patients with Barrett’s esophagus is the development of adenocarcinoma. However, only a few patients are at risk. According to epidemiological data, most patients with BE and adenocarcinoma are older white males. Patients who have specialized columnar epithelium cells are also at high risk for developing adenocarcinoma associated with BE.
An additional risk factor for metachronous and synchronous adenocarcinoma is the presence of epithelial dysplasia, especially high grade. Many studies have also indicated that the frequency of the occurrence of dysplasia, either close to or distant from Barrett’s esophagus, is also connected with adenocarcinomas.
Dysplasia is not only a sign of increased risk of adenocarcinoma but a pre-invasive lesion.
References
- https://www.cancer.org/cancer/esophagus-cancer/causes-risks-prevention/risk-factors.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861756/
- https://www.asge.org/home/for-patients/patient-information/understanding-gerd-barrett-39-s
- https://www.bmc.org/gastroenterology/high-grade-dysplasia
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4113043/
- http://pathology.uic.edu/understanding-your-report-esophagus-barretts/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4449455/