.jpg) By Chloe Bennett, B.Sc.
By Chloe Bennett, B.Sc.Dialysis is a procedure that can help patients with end stage renal disease to increase quantity and quality of life. However, there are several inherent risks associated with dialysis, which are more profound in patients at risk of complications, such as the elderly or those with other concurrent health conditions.
 Image Credits: Saengsuriya Kanhajorn / Shutterstock.com
Image Credits: Saengsuriya Kanhajorn / Shutterstock.com
What is Dialysis?
Typically, the kidneys are responsible for the removal of surplus fluid and for turning excess products into urine, which is then excreted. However, in those with impairments in kidney function, dialysis is often required. Dialysis is a medical procedure that assists in the functions usually carried out by the kidneys in those with poorly functioning kidneys, such as people with renal disease.
Without dialysis, those with kidney issues may experience a toxic build-up of fluid and waste bi-products that can have serious health implications, including death. Therefore, dialysis enables such individuals to have an improved quality of life.
There are two main types of dialysis: peritoneal dialysis and hemodialysis. For most individuals requiring dialysis, they can decide which type of procedure they would prefer as they are both equally efficacious. However, both come with their own benefits and disadvantages that need to be considered by the patient.
Peritoneal Dialysis
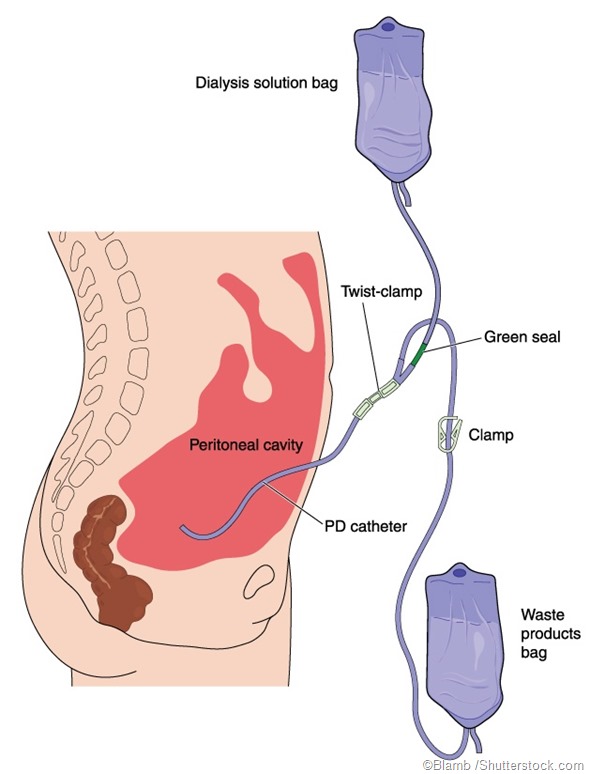
Instead of using a machine to carry out dialysis, peritoneal dialysis (PD) utilizes the abdomen lining as the filter. The vast network of capillaries in the peritoneal and the layer of mesothelial cells form a semipermeable membrane, which makes it suitable to filter products and allows for the movement of substances.
There are two main types of PD: automated peritoneal dialysis and continuous peritoneal dialysis. Both have their advantages and their drawbacks.
In certain instances, PD will be recommended to patients such as those with some remaining renal function, in infants less than two years old, and those without comorbid health conditions such as cancer and heart issues.
Benefits
One of the main advantages of PD over hemodialysis is that the procedure can be carried out in the comfort of the patients’ home. For most, all that is required is a washroom with fresh running water, a sterile area of the house for the procedure to take place, and space to store the fluid for dialysis. This also allows patients to travel.
For elderly patients who may be unable to administer the procedure themselves, assistance may be given by a trained carer or community nurse. Additionally, the procedure can even be run while the patient sleeps.
Disadvantages
One of the most significant disadvantages of PD is that it’s required to be carried out every day, which may act as an inconvenience for some. Furthermore, by undergoing PD specifically, there may be a greater risk of developing peritonitis – an infection of the abdomen.
In some, quite rare instances, patients may experience scarring and thickening of the peritoneum. In order to prevent this, patients may have to change their treatment to hemodialysis.
Additionally, those who undergo PD may report increased fatigue and malnutrition caused by the dialysis fluid, which can lower protein levels.
Automated PD and Continuous PD
Automated PD may be preferred by patients.
There are a few contraindications for PD. Those that have been diagnosed with inflammatory bowel disease or have recently undergone surgery to artificially open an organ, such as a stoma or colostomy, may be unsuitable for PD. This is due to the potential increase in the risk of infection or leak. Furthermore, PD might not be recommended in cases where the individual is unable to carry out the process themselves. For example, those generally in poor health, those with dementia-related disorders, and those with visual impairments.
Finally, potential discomfort may arise in some patients due to having a permanent catheter.
Haemodialysis
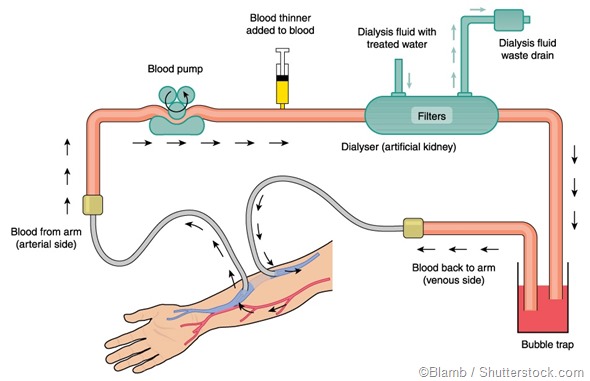
Haemodialysis is the most recognized and commonly used type of dialysis. During the procedure, a tube is connected to the patient’s arm via a needle. The blood travels through the tube to an external machine that is comprised of a dialyzer – a filter that has a semipermeable membrane. The machine creates a gradient of counter-current flow that enables the blood and the dialysate fluid to travel in opposing pathways. Waste products are then removed from the blood and passed to the dialysate fluid.
Benefits
In comparison to PD, one of the major benefits of hemodialysis is that it enables patients to have four days per week where treatment is required. This arguably can further improve patients’ quality of life by giving them more freedom.
Disadvantages
In contrast to PD, one of the main disadvantages of hemodialysis is that it often requires patients to go to the hospital three times per week for sessions that last approximately four hours. However, some patients may be able to carry out hemodialysis at home.
Furthermore, for patients wanting to travel to a different country, they’d need to locate clinics or hospitals where they can undergo dialysis while away. Additionally, those choosing hemodialysis specifically may face dietary and fluid intake restrictions.
Sources
NHS. (2018). Dialysis: Overview. https://www.nhs.uk/conditions/dialysis/
Sachdeva, B., Zulfiqar H., & Aeddula N. R. (2019). Peritoneal Dialysis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK532979/
Francois, K., & Bargman, J. M. (2014). Evaluating the benefits of home-based peritoneal dialysis. International Journal of Nephrology and Renovascular Disease. DOI: 10.2147/IJNRD.S50527
Al-Natour, M., & Thompson, D. (2016). Peritoneal Dialysis. Seminars in Interventional Radiology. DOI: 10.1055/s-0036-1571804
NHS (2018). Dialysis: How it’s performed. https://www.nhs.uk/conditions/dialysis/what-happens/
Vadakedath, S., Muacevia A., & Alfer, J. R. (2017). Dialysis: A Review of the Mechanisms Underlying Complications in the Management of Chronic Renal Failure. Cureus. DOI: 10.7759/cureus.1603
Further Reading
Last Updated: Nov 27, 2019