Skip to:

Gluten free. Image Credit: Baibaz / Shutterstock
Why a Gluten Free Diet?
Gluten is a protein found in grains such as wheat, barley, and rye, and is comprised of gliadins. For some people, eating foods that contain gluten can cause digestive problems due to gluten-related disorders.
Gluten-related disorders can range from mild to severe in symptoms, and include celiac disease and non-celiac gluten sensitivity.
For patients suffering with gluten-related disorders, it is necessary to stick to a gluten-free diet. More recently, people who do not suffer from gluten-related disorders have started to adopt a gluten-free diet as part of a lifestyle choice.
The rising popularity of gluten-free diets as a lifestyle choice means that they outnumber the number people who must eat a gluten-free diet for their gluten-related disorder.
How Does a Gluten-free Diet Affect the Microbiota?
The gut microbiota consists of the numerous microorganisms that live in our gut. It has been shown that the gut microbiota is key to protecting our gut against pathogens, and that it has the ability to make and regulate molecules going into the blood.
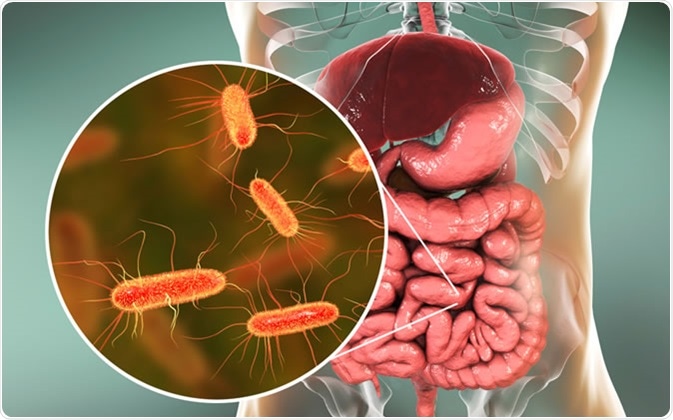
Intestinal microbiome, 3D illustration showing anatomy of human digestive system and enteric bacteria Escherichia coli, E. coli, colonizing jejunum, ileum, other parts of intestine. Gut normal flora - Illustration Credit: Kateryna Kon / Shutterstock
Also, the microbiota has the ability to process molecules that the host does not have the capacity to process. For example, the microbiota can metabolize carbohydrates that the host cannot digest, and produce vitamins that the host cannot.
It is heavily influenced by diet, therefore there have been various studies done to investigate how a gluten-free diet affects the gut microbiota.
Bonder and co. investigated the effect of a short-term gluten-free diet on the microbiota. For this study, the authors recruited 21 adult volunteers who did not suffer from symptomatic gluten-related disorders, and followed them through 4 weeks on a gluten-free diet, 5 weeks on a “wash-out” diet and a further 4 weeks on the individuals’ habitual diet.
Fecal samples were collected from the volunteers before the gluten-free diet, then weekly during the gluten-free diet and the habitual diet. DNA was then extracted from the stool samples, and the 16S rRNA sequence was determined to see the bacterial composition in the microbiome.
The authors found that while there was no difference in the overall microbiome diversity of individual volunteers, certain species changed in abundance on a gluten-free diet. This included reductions in Veillonellaceae family, Ruminococcus bromii and Roseburia faecis, and increases in Victivallaceae, Clostridiaceae and Coriobacteriaceae families. Most of these species are known to play a role in starch metabolism.
In another study, by de Palma and co., 10 volunteers without symptomatic gluten-related disorders were recruited, and over one month their diet was changed to gluten-free. When the fecal microbiota was analyzed by a combination of techniques, it showed that the number of beneficial bacteria (Bifidobacterium, Lactobacillus) decreased while numbers of potentially pathogenic bacteria (Enterobaceriaceae, E. coli) increased.
In the case of patients with celiac disease, it has been shown that their microbiota is altered: there is a decrease in protective species and an increase in species that could become pathogenic.
Initial studies showed that the imbalance in the microbiota of celiac patients was still somewhat unbalanced after 2 years on a gluten-free diet. This was noticed in the reduced number of potentially pathogenic bacteria, such as E. coli and Staphylococcus species, while the number of protective species such as Bifidobacterium and Lactobacillus was still reduced.
This has been supported by other studies, which showed a reduction in other protective species such as Enterococcus, and an increase in other potentially pathogenic species such as Bacteroides, Salmonella, Shigella, Klebsiella and Enterobacteriaceae family. These changes could also influence inflammation in the gut.
Overall, these studies show that dysbiosis of the gut microbiota seen in celiac disease patients is not fully reversed by the adoption of a gluten-free diet.
In conclusion, these studies show that a gluten-free diet can cause changes in the gut microbiota, and that this could potentially be harmful.
What are the Difficulties in Studying the Microbiota?
While there are consistent findings from these studies, there are some limitations. One limitation is that there are many ways of studying the microbiota, ranging from culture-based methods to DNA sequencing-based methods.
Each technique has its own advantages and disadvantages, and it is difficult to know if differences between these techniques can be accounted for.
Another limitation is the classification of the species in the microbiota: it is traditionally thought that bacteria belonging to the same species have highly similar DNA sequences, but this is not always the case.
Also, some studies group similar 16S rRNA sequences into “operational taxonomic units” (OTUs) based on similarity, but these OUTs may be made up of species that are not related at all.
It should also be noted that genes can pass easily between bacteria, therefore this could create species that are difficult to classify due to the presence of genes that originate from other species.
Further Reading
Last Updated: Sep 25, 2019