Multiple myeloma is a disease characterized by the proliferation of plasma cells which can lead to the abnormally high production of monoclonal immunoglobulins, detected in serum and urine. These plasma cells can enter the bone marrow and replace normal myelopoiesis. Up to 90% of patients progress to bone disease, and for this reason effective imaging is an important management technique in multiple myeloma patients.
Skip to
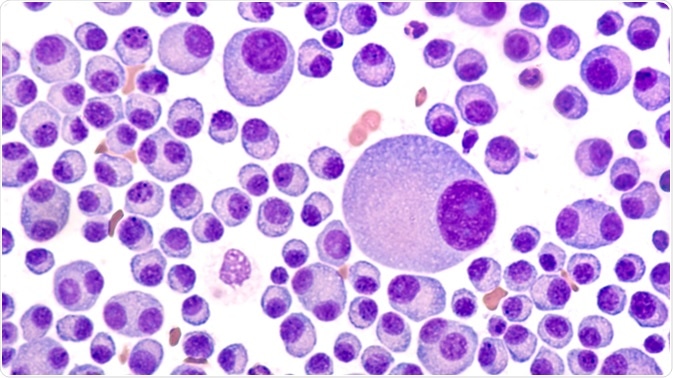
Bone marrow aspirate cytology of multiple myeloma, a type of bone marrow cancer of malignant plasma cells, associated with bone pain, bone fractures and anemia. Image Credit: David Litman / Shutterstock
Conventional radiography
Conventional radiography is the commonly used standard for diagnosis and tracking of multiple myeloma. It is currently the recommended method for most patients, and often a full conventional radiographic examination is advised for patients who have recently been diagnosed. Of these, almost 80% of patients display noticeable changes on conventional radiography.
Conventional radiography is highly effective relatively, compared to other technologies as stated, and has other advantages, too. It is widely available in many clinics and is not expensive. Furthermore, radiography can cover almost the entire skeletal system.
On the other hand, conventional radiography has low sensitivity. Lytic lesions of the bone are only picked up if over 30% of the trabecular bone is destroyed, which could mean many bone lesions go undetected. Extraosseous lesions are also often missed.
Conventional radiography is less frequently recommended for use in diagnosing and tracking multiple myeloma, due to the increased efficiency of other methods such as computed tomography and magnetic resonance imaging.
Computed tomography
Small lesions that cannot be detected using conventional radiography may be seen with computed tomography (CT). Furthermore, alterations that happen early on during multiple myeloma are more reliably detected using CT.
CT has a number of advantages over conventional radiography. For one, CT has higher sensitivity. This is especially true for areas that are overlaid on conventional radiographs, for example the ribs, the scapulae, and the sternum. Cross-sectional CT can also reveal possible instabilities and potential fracture sites with a greater chance of success compared to conventional radiography.
In healthcare settings too, CT offers several benefits over conventional radiography. CT images are generated quickly, thus improving efficiency. It also allows for examination of patients who are lying on their backs, avoiding the need for recurrent relocation which can be a great relief for patients in pain. The images acquired by CT can be used to map radiation therapy, and can also reveal extraosseous signs of multiple myeloma.
The trade-off is serious, however. The radiation dosage with a CT scan is quite high. This can be overcome by adapted low-dose CT protocols that remain effective at detecting osteolytic bone lesions. Furthermore, the sensitivity of CT is limited when it comes to the discovery of diffuse bone marrow infiltration, lytic reaction-free bone marrow lesions, and certain extraosseous lesions. Despite the limitations, whole body low-dose CT is replacing conventional radiography because of its elevated sensitivity for osseous lesions and the ability to discover extraosseous lesions.
Magnetic resonance imaging
The use of magnetic resonance imaging (MRI) for multiple myeloma has become increasingly popular due to the ease of detection of bone marrow infiltration by myeloma cells. MRI has a higher sensitivity compared to conventional radiography. In fact, focal lesions have been found using MRI in up to half of patients in whom conventional radiography failed to throw up any clear signs.
MRI is particularly effective in areas such as the skull, spine, pelvis, sternum, and scapulae. MRI has the highest sensitivity for osseous lesions, soft tissue lesions, and organ infiltrations in multiple myeloma, compared to either conventional radiography and CT.
MRI is superior to both conventional radiography and CT in terms of imaging the spinal cord and nerve roots, detecting soft tissue signs of multiple myeloma, and the ability to distinguish physiological and myeloma-infiltrated bone marrow. When there are no visible signs on an MRI, it indicates a very low tumor burden, whereas an MRI showing diffuse involvement and contrast enhancement indicates high tumor burden. MRI can give a better indication of soft tissue masses in patients who have painful myeloma.
The disadvantages of MRI relate to several important healthcare aspects. Gadolinium-based contrast agents are administered intravenously, but these could enhance the risk of progressive disease leading to nephrogenic system fibrosis. This is especially true in patients with renal insufficiency.
Furthermore, MRI has relatively high costs and a long scanning time, which can be challenging for seriously sick patients. Despite this, MRI is often recommended for the initial staging of multiple myeloma. MRI can be used in combination with CT to evaluate the presence of osteolytic lesions and to assess the stability of the disease.
Combined imaging using both PET/CT
Combined imaging techniques with PET and CT are now being used to cut down screening time and allow the acquisition of multiple parameters in the same image. Not only are osseous lesions picked up clearly, but isolated medullary lesions even when the bone is apparently normal, and extraosseous lesions, are picked up. This makes it useful in staging and monitoring some types of myeloma.
Further Reading
Last Updated: May 8, 2019