Osteoporosis is a common, yet serious bone disease affecting one-third of women and one-fifth of men worldwide. Caused by changes in the activity of bone generating and destroying cells leading to overall reduced bone mass density, this article discusses the hormonal, medication and lifestyle factors that contribute to its development.
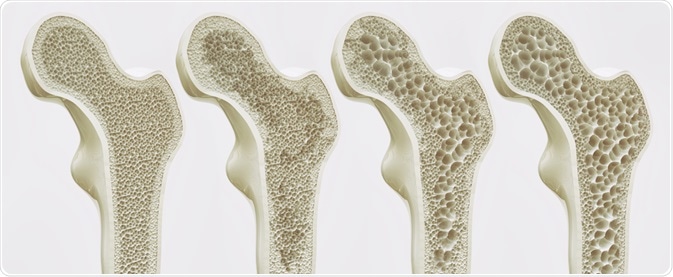 Image Credit: Crevis / Shutterstock.com
Image Credit: Crevis / Shutterstock.com
What is osteoporosis?
Osteoporosis is a systemic skeletal condition that leads to bones becoming brittle and weakened, increasing the risk of fractures. Bone is a constantly renewing living tissue, with cells called osteoblasts creating new bone material, and cells called osteoclasts destroying bone tissue.
Osteoporosis occurs when the balance between the formation of new bone tissue and the destruction of old tissue leads to reduced bone density overall. Literally translated, the term osteoporosis means ‘porous bone’. Compared to normal bone tissue which appears honeycomb-like under a microscope, osteoporotic bone is characterized by holes and spaces that are much larger than in healthy bone tissue.
The process of osteoporosis occurs slowly over several years, often only diagnosed after an impact or fall that results in a fracture. The most common fracture sites for people with osteoporosis are the wrist, hip or vertebrate, leading to permanent physical pain and loss of mobility.
Who is affected by osteoporosis?
Osteoporosis is the most common bone disease, affecting approximately 200 million people worldwide. As the incidence of osteoporosis rises with age, the increasingly aging population means that the prevalence of osteoporosis has risen sharply.
The condition affects both genders: population predictions estimate that 30% of women and 20% of men globally over the age of 50 will experience a ‘fragility fracture’ or fracture caused by osteoporosis.
What are the causes of osteoporosis?
The endocrine system
Several hormones are associated with triggering activity in osteoblast or osteoclast cells, resulting in either reduced bone formation or increased bone destruction:
Thyroxine: Hyperthyroidism (the overproduction of thyroid hormone) increases the activity of osteoclasts, speeding up the rate at which bone cells are destroyed. This occurs when the level of thyroxine in the body is elevated for a long period, or when thyroid-stimulating hormone (TSH) levels remain low for a long period.
Estrogen: Estrogen levels are strongly associated with osteoporosis in postmenopausal women and elderly men. It is associated with large levels of bone reabsorption due to increased osteoclasts. Estrogen deficiency affects the number of osteoclasts both by stimulating their production and decreasing apoptosis.
Testosterone: The most important predictor of osteoporosis in elderly men is age-related deficiencies in testosterone. Androgens (an umbrella term for testosterone and its precursors) both stimulate the production of osteoblasts and decrease their apoptosis. Androgens also regulate the formation and survival of osteoclast cells.
Cortisol: Produced by the adrenal glands, the overproduction of cortisol can have powerful effects on bone density. In patients with Cushing’s syndrome, a term used to describe a constellation of symptoms caused by an excess of cortisol, a dramatic reduction in bone density can be observed. In the elderly, weak correlations between levels of cortisol and bone density, and changes in cortisol and bone density over time have been observed.
Medications
Drug-induced osteoporosis is a significant health concern as many commonly prescribed treatments can contribute to bone loss.
Corticosteroids, which are widely used in the management of many conditions, are associated with reduced bone density. They are the second most common cause of secondary osteoporosis with as many as 50% of patients experiencing an eventual fracture if taken long-term.
Corticosteroids increase osteoblast apoptosis, increase bone reabsorption and reduce bone growth factors associated with bone regeneration. Finally, steroid use also increases calcium deficiency.
Antiepileptics which are used to treat seizure disorders induce certain enzymes that cause the body to rapidly metabolize vitamin D and estrogen. Anticonvulsants may also inhibit the absorption of calcium and increase bone loss by inhibiting the production of osteoblasts.
Heparin, an anticoagulant medication used in the treatment of pulmonary conditions, is associated with loss of bone tissue, especially longer-term use at higher doses. Although the mechanisms by which this occurs is not yet fully understood, heparin is thought to stimulate osteoclast production and inhibit osteoblast production.
Malabsorption disorders
Gastrointestinal disorders such as ulcerative bowel disease are strongly associated with secondary osteoporosis. Such disorders interfere with the absorption of nutrients essential for maintaining the balance between bone resorption and generation. Furthermore, these conditions are often treated with corticosteroids.
Lifestyle factors
A poor diet deficient in nutrients such as calcium and vitamin D is a risk factor for osteoporosis. People with eating disorders such as anorexia and bulimia nervosa are particularly at risk due to a lack of nutrient intake and hormonal changes associated with low body weight. In males and females, maintaining a low body weight increases cortisol production and decreases growth hormones. Females may be particularly vulnerable as low weight also inhibits the production of estrogen.
An inactive lifestyle can increase the risk of osteoporosis as weight-bearing exercise stimulates bone development and reduces calcium loss from bones. Extreme inactivity such as bed rest can cause extreme bone loss, especially in the first months.
Excessive smoking and alcohol consumption also increase the risk of bone loss and fracture by impacting on hormonal systems associated with bone production. The risk is increased if they occur in tandem with poor diet and inactivity.
References
Cannarella, R., Barbagallo, F., Condorelli, R., Aversa, A., La Vignera, S. and Calogero, A., 2019. Osteoporosis from an Endocrine Perspective: The Role of Hormonal Changes in the Elderly. Journal of Clinical Medicine, 8(10), p.1564.
Hardy, R. and Cooper, M., 2010. Adrenal gland and bone. Archives of Biochemistry and Biophysics, 503(1), pp.137-145.
Krela-Kaźmierczak, I., Szymczak, A., Łykowska-Szuber, L., Eder, P. and Linke, K., 2016. Osteoporosis in Gastrointestinal Diseases. Advances in Clinical and Experimental Medicine, 25(1), pp.185-190.
Mohamad, N., Soelaiman, I. and Chin, K., 2016. A concise review of testosterone and bone health. Clinical Interventions in Aging, Volume 11, pp.1317-1324.
Cdn.nof.org. 2020. Osteoporosis Fast Facts. [online] Available at: <https://www.bonehealthandosteoporosis.org/wp-content/uploads/2015/12/Osteoporosis-Fast-Facts.pdf> [Accessed 6 November 2020].
Riggs, B., 2000. The mechanisms of estrogen regulation of bone resorption. Journal of Clinical Investigation, 106(10), pp.1203-1204.
Riggs, B., Jowsey, J., Kelly, P., Jones, J. and Maher, F., 1969. Effect of sex hormones on bone in primary osteoporosis. Journal of Clinical Investigation, 48(6), pp.1065-1072.
Last Updated: Jul 14, 2023