Clostridium difficile, also called C. difficile or C. diff, is a bacterium that mainly infects the large intestine and causes diarrhea and other life-threatening intestinal disorders.
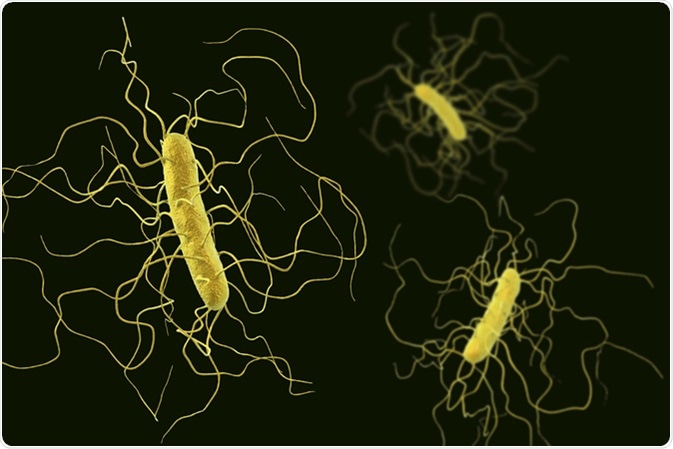
Clostridium difficile bacteria isolated on black background, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
What are the characteristics of C. difficile infection?
Clostridium difficile is a Gram-positive bacterium that induces inflammation in the intestine via two toxins, namely TcdA and TcdB. A variety of microbes (microbiota) that are normally present in the gastrointestinal (GI) tract prevent C. difficile colonization of and damage to the intestinal cells. However, weakening of the microbiota following antibiotic treatment can facilitate the overgrowth of C. diff, which is naturally resistant to common antibiotics because of its spore-forming ability.
C. diff is generally found in a dormant form in the intestine of 5 – 10% of healthy people as well as in animals such as horses, pigs, and cattle. The elderly are more susceptible to C. diff infection, usually after treatment with antibiotics, and since this is more common in hospitals and other healthcare setups, they form a distinct risk group here. People with weak immune systems or a previous history of C. diff infection are also at higher risk.
C. diff is a major source of healthcare-related infections, which spread mainly through the fecal-oral route. The spores formed by C. diff are passed in the feces of infected people and easily contaminate water, food, and other nearby objects/surfaces. The spores can survive in the environment for several weeks or months and cannot be destroyed by common chemical cleaning agents such as hand sanitizers. The infection is spread from person to person by touching the contaminated surfaces.
Clostridium difficile (c.diff) Infection | Clostridioides difficile infection | GI Society
What are the common signs and symptoms of C. diff infection?
The signs and symptoms of C. diff infection vary with its severity. There are C. diff carriers who carry the organisms in their intestines but never develop infection. People with mild to moderate infection mostly complain of watery diarrhea (at least 3 times a day for two or more days), abdominal pain, and stomach tenderness.
In case of severe infections, severe diarrhea (10 – 15 times a day) is often present with dehydration, and may require hospitalization. Such infection also causes colon inflammation (colitis), which sometimes results in bleeding and pus formation (pseudomembranous colitis). People with severe infection frequently complain of severe abdominal pain associated with fever, a rapid heart rate, and kidney problems.
Because of GI tract effects, these individuals experience nausea and loss of appetite, which can lead to severe weight loss. In some cases, blood or pus may be passed in the stool, which is a sign of worsening.
What are the risk factors for C. difficile infection?
Although C. diff infection can affect people with no obvious susceptibility, the presence of certain factors increases the risk of infection. One of the major risk factors is prolonged or recent consumption of broad-spectrum antibiotics or multiple antibiotics. In addition, medicines that are used to prevent acid reflux, such as proton pump inhibitors, can increase the risk of developing C. diff infection.
Another major risk factor is exposure to the healthcare setups, such as hospitals, nursing homes, and long-term care facilities. People admitted to these setups are more susceptible to infection because of frequent antibiotic use and easy transmission of bacteria.
People with serious illnesses such as inflammatory bowel syndrome or colorectal cancer are at higher risk of developing C. diff infection. Moreover, people who have undergone abdominal surgeries or gastrointestinal diagnostic procedures are more susceptible.
Age is another important risk factor for C. diff infection. People aged 65 years or older are 10 times more likely to develop the infection compared to younger people. In addition, a previous history of C. diff infection can increase the risk of recurrence by up to 20%.
How is C. diff infection treated?
The diagnosis of C. diff infection is mainly performed by stool examination. However, the detection of particular bacterial strains is performed by specialized methods, such as polymerase chain reaction (PCR).
Because of a high recurrence rate, the treatment of C. diff infection is often difficult. The infection is primarily treated by antibiotics; however, in some very severe cases, surgery is performed to remove the affected part of the intestine.
How can C. diff infection be prevented?
Several measures can be taken to prevent the spread of C. diff. For example, healthcare providers should wash their hands with soap and water before and after treating infected people. Visitors who come to see patients in the hospital should also wash their hands carefully before and after every visit.
Since commonly used cleaning products cannot destroy C. diff spores, all surfaces that are adjacent to an infected person should be carefully cleaned with chlorine bleach. People infected with this organisms must stay away from childcare facilities and all kinds of schools as well as from work for at least 24 hours from the stop of diarrhea. If the job contains food handling, diarrhea and vomiting must clear for at least 48 hours before returning to work.
The most important measure to prevent C. diff infection is to stop unnecessary use of antibiotics. In case of absolute necessity, doctors should prescribe narrow-range antibiotics for the shortest duration possible.
The Gut Microbiome and C. difficile
Further Reading
Last Updated: Mar 18, 2019