Morton’s neuroma, also known as Morton’s metatarsalgia or interdigital neuroma, is a health condition that involves perineural fibrosis and degeneration of the common digital nerve in the foot.
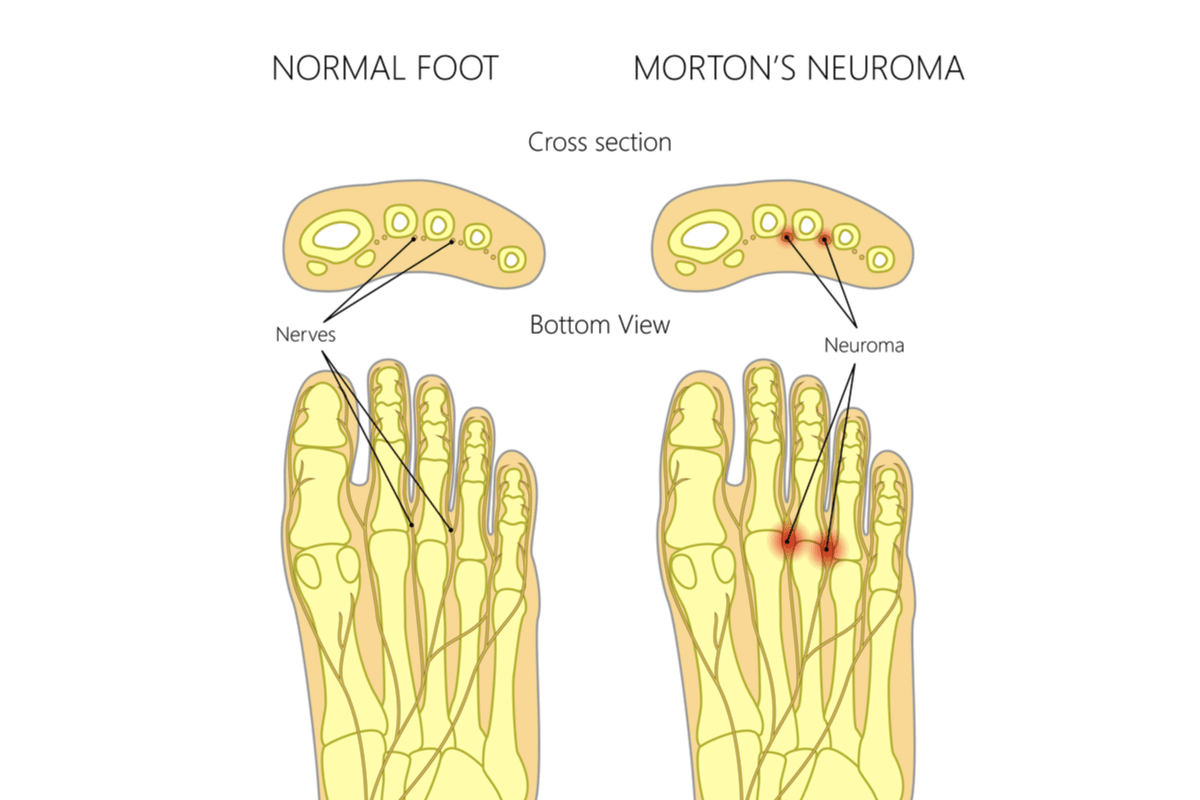
Image Credit: Aksanaku / Shutterstock.com
Morton's neuroma results from irritation or thickening of one nerve, which can cause severe pain between the toes or on the ball of the foot. This condition was first described in 1876 and is not a true neuroma, despite resulting in neuropathic pain.
Morton's neuroma can affect anyone of any gender and age; however, it is most common among middle-aged women, with a female to male ration of 5:1. This increased prevalence in women has been linked to the style of footwear often worn by these women that put additional pressure and stress on the feet. It is also more common among people that participate in high-impact sports.
Causes
Morton’s neuroma presents as the result of irritation or thickening of a plantar digital nerve located between the toes in the foot. The primary causes of Morton's neuroma usually involve compression, stretching or damage to the nerves and can include:
- Wearing ill-fitting shoes (e.g., tight, pointed-toe or high-heeled shoes)
- Participating in high-impact sporting activities (e.g., running and racquet sports)
- Abnormalities of the foot structures (e.g., flat feet, high arches, bunions or hammertoe)
However, it is unclear if these factors directly cause Morton’s neuroma, or if they increase the risk of an individual who is already susceptible to the disease to experience symptoms.
Symptoms
The primary symptom of Morton’s neuroma is severe pain between the toes or at the base of one or both feet, which can prevent them from moving normally in some cases. Morton's neuroma usually affects the area between the third and fourth toes;; however, other nerves can be affected.
Patients with Morton's neuroma often report a tingling sensation initially, which gradually worsens until it becomes severe and is subsequently described as a sharp, shooting or burning pain. Some patients also report a lack of sensation and numbness in their feet, while others describe the pain to be similar to walking with a pebble in their shoe.
The pain associated with this condition usually increases in intensity during activities that place pressure on the feet, such as walking or wearing tight-fitting shoes. Conversely, symptoms usually improve if the patient is able to rest or remove the ill-fitting shoes.
Patients may have a flare-up with frequent symptoms present over a period of a few weeks, followed by another period of remittance with no evidence of symptoms. In fact, some patients may go up to a year without experiencing symptoms, although the attacks tend to increase in frequency with time.
Diagnosis
Individuals who report symptoms of Morton’s neuroma should seek medical advice about the appropriate treatment, as the condition is usually chronic and will not subside spontaneously.
The patient consultation should involve a discussion about the symptoms, including the:
- Initiation and duration of symptoms
- Description and progression of pain
- Personal risk factors (e.g., types of shoes worn during work or sports activities)
A physical examination and motion tests can be used to diagnose the condition. In some cases, further diagnostic tests such as X-ray imaging may be required.
What is Morton's Neuroma? Symptoms, Treatments and More!
Treatment
The initial treatment of Morton’s neuroma usually involves simple lifestyle changes to eliminate the likely cause of the condition. This may include an avoidance of wearing ill-fitting shoes, using orthoses to support the foot or reducing participation in high-impact sporting activities. Corticosteroid injections can also help to reduce the pain and inflammation of the nerve in order to relieve some of the symptoms.
For over 80% of Morton's neuroma cases, these non-surgical techniques are able to provide sufficient relief. However, some patients will require surgical treatment to resect a portion of the nerve or release some of the surrounding tissues to relieve symptoms.
References
Further Reading
Last Updated: Mar 18, 2021