Oxygen saturation is a measure of the amount of hemoglobin that is bound to molecular oxygen at a given time point. It is an important parameter for managing patients in a clinical setup.
 Image Credit: Juan R. Velasco/Shutterstock.com
Image Credit: Juan R. Velasco/Shutterstock.com
What is oxygen saturation?
Oxygen saturation measures the percentage of oxyhemoglobin (oxygen-bound hemoglobin) in the blood, and it is represented as arterial oxygen saturation (SaO2) and venous oxygen saturation (SvO2). Oxygen saturation is a vital parameter to define blood oxygen content and oxygen delivery.
Each hemoglobin molecule contains four heme groups that can readily bind molecular oxygen present in the blood. This means that a hemoglobin molecule can bind up to four oxygen molecules during transport in the blood.
For adults, the normal range of SaO2 is 95 – 100%. A value lower than 90% is considered low oxygen saturation, which requires external oxygen supplementation.
During aerobic metabolism, the body utilizes oxygen to convert glucose into pyruvate and generate two molecules of ATP. The oxygen content in the blood depends on the oxygen-hemoglobin dissociation curve, which is a plot to define the percentage of saturated hemoglobin to the partial pressure of oxygen (PO2). A hemoglobin molecule becomes 100% saturated with oxygen (1.34 L of oxygen) at a PO2 of 100 mmHg.
After binding each oxygen molecule, hemoglobin undergoes a conformational change that increases its affinity for the next oxygen molecule. Because of the high oxygen affinity, each hemoglobin molecule becomes rapidly saturated with oxygen; thus, the amount of free oxygen dissolved in the blood is only a very small fraction (2%) of the total oxygen present in the blood. Because of this, the level of oxyhemoglobin is considered equal to the blood oxygen content.
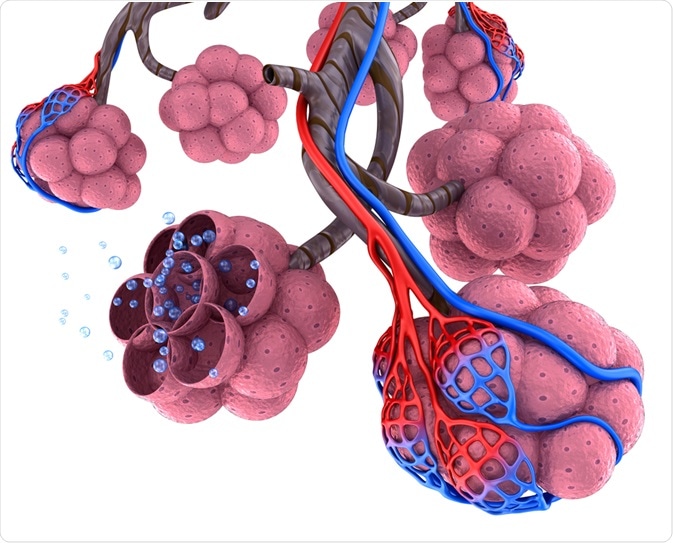
Image Credit: Alex Mit/Shutterstock.com
How to measure oxygen saturation in the blood?
Measurement of oxygen saturation is particularly important for patients with health conditions that can reduce the level of oxygen in the blood. These conditions include chronic obstructive pulmonary disease (COPD), asthma, pneumonia, lung cancer, anemia, heart failure, heart attack, and other cardiopulmonary disorders.
The most common method of measuring oxygen saturation is pulse oximetry. It is an easy, painless, non-invasive method wherein a probe is placed on the fingertip or earlobe to measure the oxygen saturation indirectly.
The probe uses 2 light sources, red light, and infrared light, which are absorbed by the blood. Higher absorption of infrared light indicates good oxygen saturation, whereas a higher absorption of red light indicates poor saturation. Readings obtained from a pulse oximeter are expressed in percentage.
A blood gas test is another approach to accurately measure the level of oxygen and carbon dioxide in the blood. For the test, the blood can be collected from the wrist (arterial blood gas test) or earlobe (capillary blood gas test). This test is mainly used to determine if the lungs are fully functional to exchange oxygen and carbon dioxide effectively.
For the test, a small amount of blood is taken from the patient and analyzed in a portable blood gas analyzer, which provides information on oxygen, carbon dioxide, and pH levels in the blood. A patient with COPD will have reduced oxygen and pH levels and increased carbon dioxide levels in the blood.
What happens when oxygen saturation drops?
A lower than normal level of oxygen in the blood is defined as hypoxemia. Generally, an oxygen saturation level of lower than 90% is considered as hypoxemia, which can result from cardiopulmonary complications, sleep apnea, certain medicines, and high-altitude exposure.
The most common symptoms of hypoxemia include headache, rapid heart rate, coughing, shortness of breath, wheezing, confusion, and blueness of the skin and mucus membranes (cyanosis).
Cyanosis is a pathological condition characterized by extremely low oxygen saturation. There are two types of cyanosis: central cyanosis and peripheral cyanosis. In central cyanosis, oxygen saturation level drops below 85%, which causes the appearance of a bluish hue all over the skin and visible mucosa.
In peripheral cyanosis, which commonly occurs due to increased oxygen uptake by the peripheral tissues, a bluish hue appears only on the peripheral body parts, such as hands and feet. The most common causes of peripheral cyanosis include venous stasis, low cardiac output, or extreme cold exposure.

Image Credit: Zay Nyi Nyi/Shutterstock.com
How to improve low oxygen saturation?
A drop in oxygen saturation below the critical level should be treated with oxygen supplementation. Depending on the severity of the condition, a physician can prescribe supplemental oxygen, which has the most direct effect on the oxygen saturation level.
However, for mild-to-moderate conditions, there are natural ways to increase the level of blood oxygen saturation. For example, a daily physical exercise can improve the lung capacity for gaseous exchange and protect against hypoxemia. However, it is important to consult a physician before starting any exercise regimen or implementing changes in daily exercise routines.
Eating a healthy and balanced diet can also help improve blood oxygen saturation. Since iron deficiency is one of the major causes of low oxygen saturation, eating foods that are rich in iron, such as meat, fish, kidney beans, lentils, and cashew nuts, can be helpful.
References
Further Reading
Last Updated: Feb 25, 2021