Over the past decade, there has been a growing body of research that has sought to understand the complex role the microbiome plays in disease regulation. The results of these studies have brought us closer to understanding these processes and have thrown light on the complexity of the immune system.
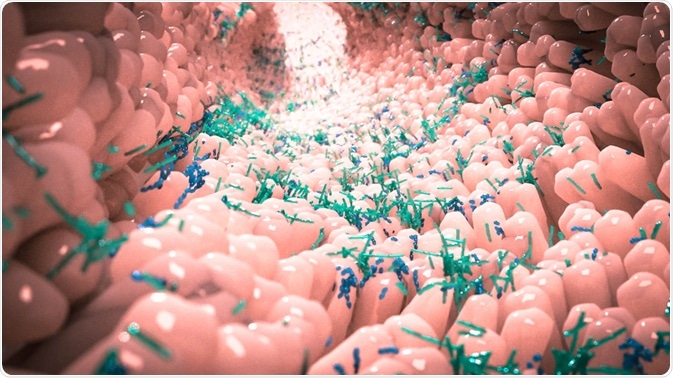
Image Credit: Alpha Tauri 3D Graphocs/Shutterstock.com
The Microbiome
The term “microbiome” refers to the bacteria present in an environment, including the Human body. Microbe populations in the body represent a major amount of biomass, with bacteria numbering in the trillions being present at any one time. The microbiome plays various functions in the body, including digestion and immunomodulation.
Research into how the Human body acquires its microbiome is subject to heated debate: whilst some studies contend that the mother passes beneficial bacteria to the fetus through the placenta, other recent studies have provided evidence that the microbiome is only acquired by a baby at birth. A study in 2014 by Marcus C. de Goffau et. al suggested that the placenta, whilst providing essential elements for life such as food and oxygen, does not itself contain a microbiome. Microbial niche specificity has been shown to exist in an infant from 6 weeks of age.
By far the largest population of microbes exists in the gastrointestinal tract, which includes the intestines and colon. Present in both the lumen and on mucosal surfaces, this is a massive reservoir of bacteria which aid in metabolism, interacting with the host’s immune system. Other populations of bacteria exist within bodily systems such as the respiratory system and on the dermal surface, carrying out specific functions and interacting with the body in their ways.
The microbiome can change its composition over time as the host organism ages and can be affected in both beneficial and negative ways by factors such as environment, diet, genetics, antibiotics, and disease.
The microbiome’s role in the immune system and disease susceptibility
Multiple studies have shown that the microbiome plays an important part in the complex interactions of the immune system. Several factors can contribute to the health of the microbiome. For example, on the skin, factors such as pH balance and substrate availability correlate strongly with the propagation of habitat-specific microbiome compositions in healthy individuals.
Factors that affect the gut microbiome include age, antibiotics, diet and living environment. The human gut microbiome reacts rapidly to dietary changes, although the dominant force in determining its composition is the long-term dietary habits of the host.
The microbes present in the gut drive immunomodulation, which has been well-understood for some time, but more recent studies have shown that the gut microbiome can influence other parts of the body including remote organs that are unconnected to the gastrointestinal system. It can also influence the mucosal and hematopoietic immune functions of the host. Considerable effort is currently being concentrated on understanding how the microbiome develops over time, in parallel with the host-microbiome molecular interactions
One of the major ways that the microbiome, especially that contained within the gut, can affect disease susceptibility is by modulating the body’s inflammation response, an important immune response pathway that can affect several conditions including type 2 diabetes and infections by a variety of pathogens. Any perturbation to the gut microbiota, for example, agitation caused by diets rich in fat and sugar, can lead to effects on inflammatory regulation.
Perturbation to the function and composition of the gut microbiota is also associated with a variety of respiratory illnesses. Factors that can affect the respiratory microbiome also affects chronic respiratory conditions. Factors that can affect this part of the body’s microbiome include smoking and environmental pressures (such as air pollution.)
Overall, the microbiome is a complex and still poorly understood system which plays an important part in immunoregulation.
In conclusion, the microbiome plays a complex role in the body’s ability to resist infection and cope with a variety of conditions. Understanding the host-microbiome interaction is integral to understanding how the body fights disease and will influence how public health policies and the drug industry play their part in the overall health of the human host.
Sources
de Goffau, M.C et al. (2019) Human placenta has no microbiome but can contain potential pathogens Nature vol. 572, pgs. 329–334
https://doi.org/10.1038/s41586-019-1451-5
Durack, J. and Lynch, S.V. (2018) The gut microbiome: Relationships with disease and opportunities for therapy, Journal of Experimental Medicine 216 (1) 20-40
https://doi.org/10.1084/jem.20180448
Edwards, S.M. et al (2017) The maternal gut microbiome during pregnancy, MCN, The American Journal of Maternal/Child Nursing. 42(6):310–317
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5648614/
Chu, D.M. et al. (2017) Maturation of the infant microbiome community structure and function across multiple body sites and in relation to mode of delivery, Nature Medicine vol. 23, pgs. 314–326
https://doi.org/10.1038/nm.4272
Last Updated: Jan 17, 2020