Nephrotoxicity is defined as the rapid deterioration in kidney function as a result of medications and chemicals. Nephrotoxicity can also be defined as an adverse event caused by substances that caused damage to renal function. These substances can include molds and fungi, cancer therapeutics, and antibiotics, metals such as arsenic, lead, and mercury, as well as drugs of abuse.
Kidneys. Image Credit: crystal light/Shutterstock.com
A hallmark indication of nephrotoxicity is an alteration in the function of the kidney. This is assessed by the glomerular filtration rate (GFR), blood urea nitrogen, urine output, and serum creatinine.
Despite these indications, some nephrotoxicants, defined as substances that induce nephrotoxicity, can induce kidney damage without altering any of these clinical markers of renal function.
The Mechanism of Kidney Injury Caused by Drugs and Their Metabolites
Drugs are typically metabolized in the liver, the gut, and the kidneys. There are two pathways for the excretion of drugs: renal and extrarenal
The renal excretion of a drug can essentially be divided into three processes: glomerular filtration, tubular reabsorption, and tubular secretion. Tubular Secretion allows the drugs to be transported from the blood to the urine via the tubular cells.
Apical contact with the compounds secreted into the tubular lumen causes the proximal tubules to be exposed; moreover, uptake by the tubular epithelial cells, or their apical efflux (movement of the substance from the region of the plasma membrane located at the apex of the epithelial cell) from the basolateral areas of the tubular cells into the tubular lumen can result in damage.
These nephrotoxic compounds are excreted from the body via glomerular filtration and tubular secretion traffic from the proximal tube into the loop of Henle. After this, they move into the distal tubule where the drugs can precipitate, crystalize, or form casts. This obstructs the tubules and causes tubular injury, which leads to acute tubular necrosis. Tubular obstruction by crystals or casts can also occur, and finally, interstitial nephritis can be induced.
Mechanisms that cause nephrotoxicity include:
- Glomerular hemodynamics: Glomerular filtration rate (GFR)is 120 ml per minute in healthy adults. Kidneys can maintain a constant filtration rate and the rate of urine production by regulating the blood flow in both the afferent and efferent arteries. The rate of blood flow affects intraglomerular pressure which drives this process. Because prostaglandins and angiotensins are used to expand the afferent arteries, anti-prostaglandin drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), drugs that have anti angiotensin activity such as angiotensin-converting enzyme inhibitors (ACEIs), or angiotensin receptor blockers (ARBs) can cause nephrotoxicity in the glomerulus
- Tubular cell toxicity: tubular cells are exposed to a toxic substance (nephrotoxin). Because renal tubules, especially proximal tubule cells, come into contact with drugs in the process of concentration and reabsorption through the glomerulus, they are prone to drug toxicity Damaged mitochondria present in the tubular cells, combined with a disturbing tubular transport system, and an increase in oxidative stress by free radical production causes cytotoxicity. Drugs that are known to induce cytotoxicity include aminoglycoside antibiotics, anti-fungal drugs, anti-retroviral drugs come out and anti-cancer drugs.
- Inflammation: Inflammation can be induced by nephrotoxins. This causes fiberization of the kidney tissue. This subsequently causes glomerulonephritis, and acute and chronic interstitial nephritis. Nephritis is a condition in which the nephrons, the functional units of the kidneys, become inflamed Acute interstitial nephritis is induced by NSAIDs and antibiotic drugs. Chronic interstitial nephritis is related to the long-term use of some anti-cancer drugs, analgesics, and calcineurin inhibitors.
- Crystal nephropathy: Crystals formed by drugs and their metabolites can trigger the deterioration of kidney function. The acidity of the urine affects the formation of the insoluble crystals. Drugs that can cause crystals to form include antibiotics and antiviral agents.
- Rhabdomyolysis: The breakdown of muscle tissue that leads to the release of muscle fiber contents into the blood. This causes renal muscle cells to disintegrate, causing myoglobin and serum creatine kinase to be released into the blood. Released myoglobin causes reduced filtration in the kidney, subsequently causing acute tubular necrosis or renal failure. Rhabdomyolysis typically occurs as a result of abusing drugs such as heroin, methamphetamine, methadone, and alcohol.
- Thrombotic microangiopathy: thrombosis in capillaries and arterioles, as a result of damage to the endothelium. Platelet agents have been shown to cause this.
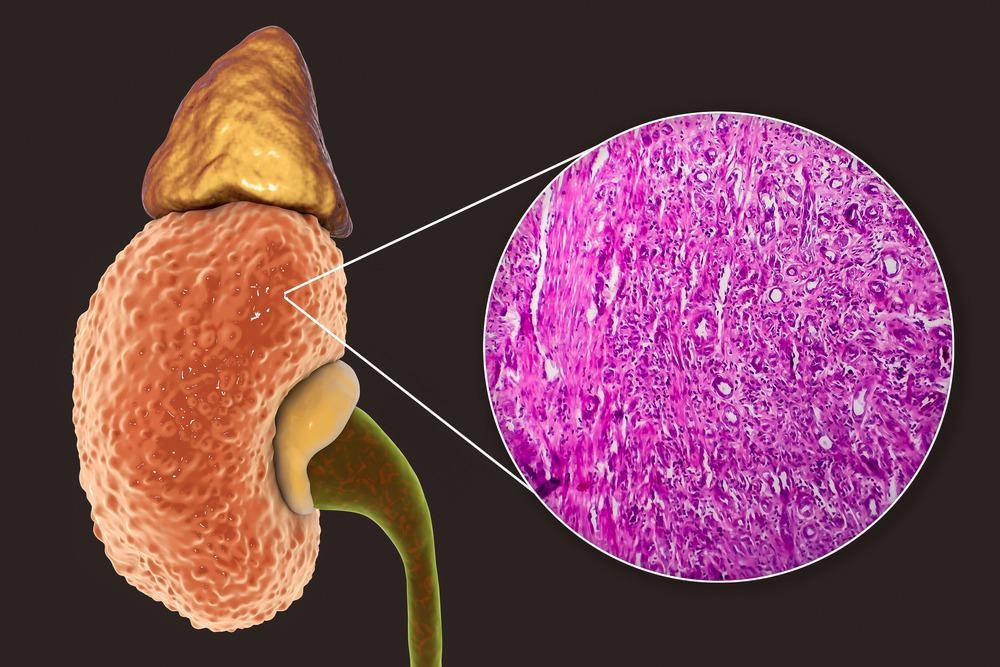
Chronic glomuleronephritis. Image Credit: Kateryna Kon/Shutterstock.com
Biomarkers to Assess Nephrotoxicity
The traditional standard markers of glomerular filtration rate (GFR), blood urea nitrogen, urine output, and serum creatinine are considered to be poorly sensitive and specific. This results in delayed diagnosis of nephrotoxicity come out with subsequent delays in treatment. Consequently, new biomarkers are necessary for the specific diagnosis of nephrotoxicity.
Biomarkers are defined as biomolecules that reveal a relationship between a substance and a disease. Generally, they enable early detection of damage to health caused by exposure to exogenous toxic substances. They also provide a basis for understanding the mechanism of the onset. Considerable progress has been made to identify biomarkers. Novel biomarkers of nephrotoxicity include:
- N-acetyl-glucosaminidase (NAG)
- Glutathione-s-transferase (GST)
- Gamma-glutamyl transpeptidase (GGT)
- Alanine aminopeptidase (AAP)
- Lactate dehydrogenase (LDH)
- Kidney injury molecule 1 (KIM-1)
Drug-induced nephrotoxicity is associated with acute and chronic renal damage as well as chronic kidney disease come out which is the major clinical manifestation of nephrotoxicity. Despite advances in the determination of biomarkers for the detection of nephrotoxicity, current kidney injury biomarkers are inadequate. A more comprehensive understanding of the biochemical pathways that leads to nephrotoxicity is necessary to provide valuable insight into the detection, monitoring, and treatment of nephrotoxicity and its clinical manifestations.
References
- Kim SY, Moon A. (2012) Drug-induced nephrotoxicity and its biomarkers. Biomol Ther (Seoul). doi:10.4062/biomolther.2012.20.3.268.
- Al-Naimi MS, Rasheed HA, Hussien NR, et al. (2019) Nephrotoxicity: Role and significance of renal biomarkers in the early detection of acute renal injury. J Adv Pharm Technol Res. doi:10.4103/japtr.JAPTR_336_18.
- Awdishu L, Mehta RL. (2017) The 6R's of drug induced nephrotoxicity. BMC Nephrol. doi:10.1186/s12882-017-0536-3.
Further Reading
Last Updated: Jun 1, 2022