Tumors are often considered to be malignant cells that operate independently of their environment; however, this is not the case.
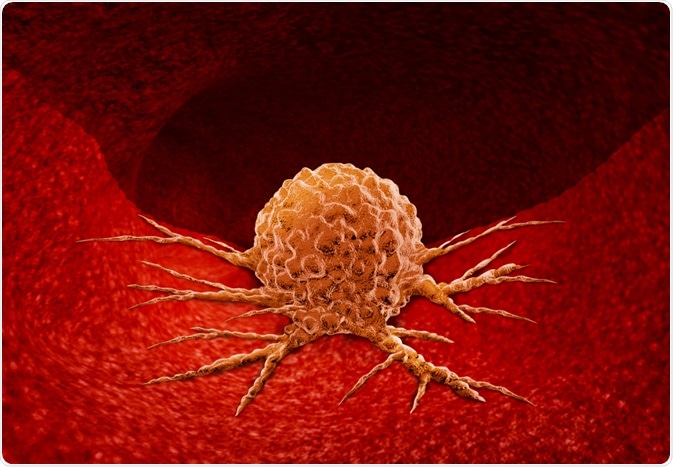
Image Credit: Lightspring/Shutterstock.com
They are entities that negatively impact their surrounding environment, corrupting and recruiting non-malignant cells in the area, resulting in the formation of what’s known as a tumor microenvironment (TME).
The TME refers to the area surrounding the tumor that encompasses surrounding blood vessels, fibroblasts, immune cells, signaling molecules, the extracellular matrix, resident and infiltrating host cells, secreted factors, proteins, tumor vasculature and lymphatics, pericytes and sometimes adipocytes.
The tumor interacts closely with the surrounding microenvironment, which is known to profoundly impact tumor progression by influencing processes that lead to tumor eradication, increased metastasis, or the establishment of dormant micrometastases.
The TME affects the therapeutic response and resistance of the tumor, which is why new therapies are being developed to target specific components of the environment. Currently, much research and development are being conducted to further understand the relationship between different kinds of tumors and the TME to establish effective new treatments.
Below, the major components of the TME of most human cancers are discussed with relevance to their importance to cancer development, spread, and treatment response.
Adipocytes
In intra-abdominal tumors that metastasize to the omentum, and some other types of tumor, adipocytes in the TME have been found to assist the recruitment of malignant cells through the secretion of adipokines, as well as promote the growth of these cells by providing them with fatty acids.
B lymphocytes
Studies have shown that B cells are sometimes found at the invasive margin of tumors, although they are most often associated with the draining of the lymph nodes as well as the lymphoid structures next to the TME. Research suggests that the infiltration of B cells in the TME is linked with a good prognosis for breast and ovarian cancer.
T lymphocytes
T cells are usually antigen ‘experienced’ and able to kill tumor cells, the presence of them is, therefore, strongly associated with a good prognosis. The existence of γδ T cells in the TME has been linked with potent cytotoxic activity against several malignant cells, such as cancer stem cells.
However, experimental evidence has been unable to prove whether the existence of γδ T cells in the TME is associated with a good or bad prognosis.
Cancer-associated fibroblasts
The normal function of fibroblasts is to stimulate organ fibrosis in response to injured tissue. However, the presence of fibroblasts in the TME has been seen to enhance the risk of cancer development.
Dendritic cells (DCs)
The normal function of DCs is to process antigens, but, those found within the TME are assumed to be malfunctioning and cannot effectively initiate the immune response to tumor-associated antigens. Further to this, some DCs have been found to act as T cell suppressors, further negatively impacting prognosis.
Lymphatic endothelial cells
Tumors generate VEGFC or VEGFD, which stimulates lymphangiogenesis. This results in lymphatic vessels sprouting in the TME along with an increased number of lymphatic endothelial cells that support the dissemination of malignant cells.
There is also a growing body of evidence that suggests the lymphatic endothelial cells mechanically modulate the TME by amending the host immune response to the tumor.
Myeloid-derived suppressor cells (MDSCs)
MDSCs are inhibitory immune cells that show increased expression in many human cancers. They are thought to inhibit the activity of T cells, which indirectly worsens prognosis.
NK and NKT cells
Natural killer (NK) cells and natural killer T (NKT) cells are considered to predict a good prognosis when they are found in the TME of colorectal, renal, gastric, liver, and lung cancers. Although, some studies suggest that NK cells may not be able to fulfill their tumor-killing function when in the TME, finding that their anergic phenotype is activated when in the presence of malignant cell-derived transforming growth factor-beta (TGF-β).
Pericytes
Pericytes are perivascular stromal cells that are known to be vital to the tumor vasculature, which provides the blood vessels with structural support. Research has proven that low pericyte coverage of the vasculature, in cancers such as colorectal and bladder, is related to increased risk of metastases and of the tumor worsening over time.
Tumor-associated macrophages (TAMs)
TAMs usually exert a pro-tumorigenic effect, inducing invasion, malignant cell migration, and metastases in most human cancers. Pre-clinical and clinical data support the idea that an abundance of TAMs in the TME is related to poor prognosis.
Tumor-associated neutrophils (TANs)
While some studies have concluded that TANs contribute to primary tumor metastasis and growth, others are skeptical. Some research has found that TANS contribute to increased angiogenesis and a reduced immune response, while others have reported cytokine activation leading to an antitumor function of TANs.
Vascular endothelial cells
Endothelial cells and their associated pericytes are often stimulated by the VEGFs, platelet-derived growth factors (PDGFs), FGFs, and chemokines present within the TME. This process supports cancer growth and can lead to the production of angiogenic factors, further enabling the development of the tumor.
Sources
- Balkwill, F., Capasso, M. and Hagemann, T. (2012). The tumor microenvironment at a glance. Journal of Cell Science, [online] 125(23), pp.5591-5596. https://jcs.biologists.org/content/125/23/5591
- Joyce, J. and Pollard, J. (2008). Microenvironmental regulation of metastasis. Nature Reviews Cancer, 9(4), pp.239-252. https://www.ncbi.nlm.nih.gov/pubmed/19279573?dopt=Abstract
- Wang, M., Zhao, J., Zhang, L., Wei, F., Lian, Y., Wu, Y., Gong, Z., Zhang, S., Zhou, J., Cao, K., Li, X., Xiong, W., Li, G., Zeng, Z. and Guo, C. (2017). Role of tumor microenvironment in tumorigenesis. Journal of Cancer, [online] 8(5), pp.761-773. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5381164/
Further Reading
Last Updated: Feb 6, 2020