Biomaterials are materials used to build medical devices or implants/prostheses, meant to restore or replace lost or impaired body functions. They are derived from natural, synthetic or semi-synthetic (also called hybrid) materials.
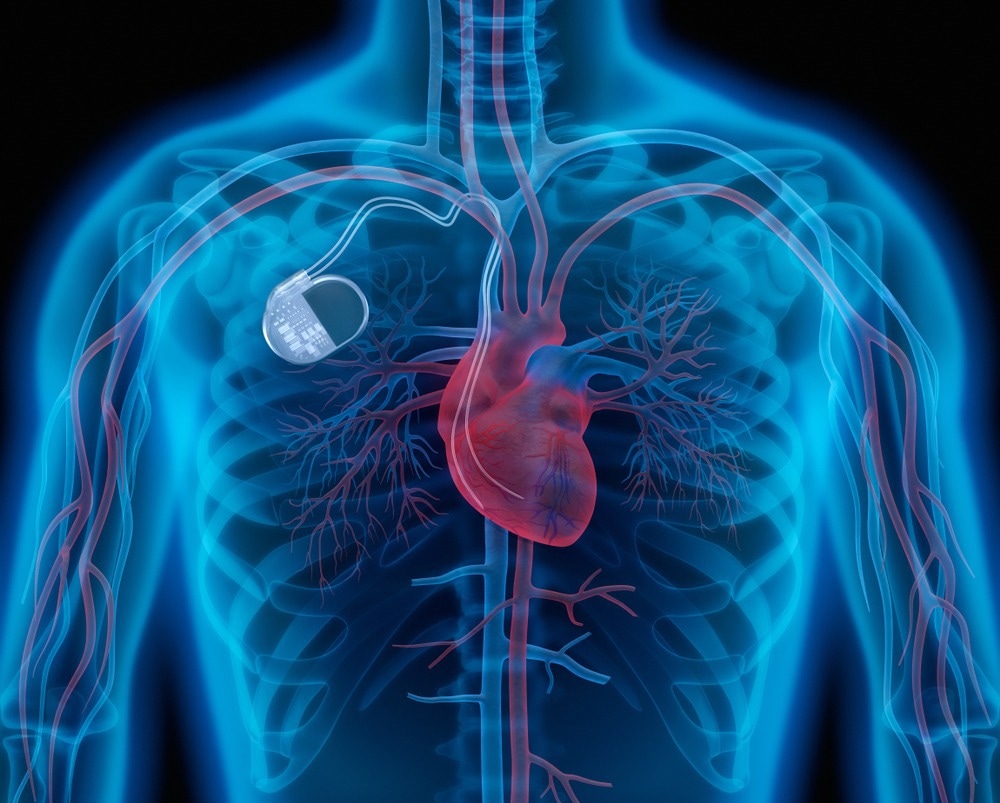
Pacemakers use biomaterials. Image Credit: peterschreiber.media/Shutterstock.com
Over 6,000 types of medical devices have been approved by the US Food and Drug Administration (FDA). These include pacemakers, plates for bone repair, artificial heart valves, and hip/knee prostheses. All of these require biomaterials to be used.
However, biomaterials have been in use since ancient times, from Rome to Etrusca.
Following the Second World War, biomaterials were developed on a much faster scale, in parallel with the explosion in materials sciences. As science and technology advanced, this field began to show marked expansion, with materials being refined to be compatible with the specific demands of the body part to be repaired or compensated for.
Another major use of biomaterials is in the manufacture of biosensors. Biosensors are being used everywhere to monitor biomarkers and to detect many conditions like type 2 diabetes.
Types
A. Natural
Natural materials include starch, collagen, bone or chitosan, while synthetic materials are created in laboratories from metals, polymers and ceramics. Hybrid materials use both types of materials. These are chosen to be biomaterials because of their combination of physical, chemical, biological and mechanical properties, by which they are suited for proper function and human body applications.
Metallic and non-metallic biomaterials are of various types, bonded covalently, ionically or both ways.
Cell therapy is a new and emerging approach to the repair of a damaged heart. Tissue engineering can create cardiac patches, modified and seeded with bone marrow or mesenchymal stem cells to form a near-natural repair. Natural and synthetic biomaterials are being explored in this area as well.
Osseoinduction is becoming a preferred technique for bone repair, using surface modification, or introducing growth factors or bone marrow stem cells into the damaged area, for instance, to induce new bone growth. This could accelerate bone healing without painful and extensive surgery.
Bone marrow stem cells are potentially very useful for skin tissue engineering, while mesenchymal stem cells may give rise to ligament fibroblasts. Fat-derived stem cells may enhance both collagen synthesis and the movement of skin fibroblasts in wounded tissue, promoting rapid wound closure.
B. Synthetic
1. Bioceramics
Bioceramics are being widely used in hip replacement, for bone grafts, dental implants, and to create artificial tendons. Black pyrolytic carbons are unsuitable for externally visible implants, as in the mouth, but are easy to manufacture and highly compatible with the body’s tissues. They are in use for heart valves, ligaments and tendons, and in composite implants, all of which require great tensile strength.
Additionally, bioceramics are being investigated as delivery vehicles for drugs, genes (for gene therapy) and cancer treatment.
Bioceramics are biocompatible, non-carcinogenic, non-inflammatory, non-allergenic and non-toxic. They are also pleasing to the eye and can be tinted to any desired color, while their compressive strength is high. They are also resistant to corrosion and make excellent articulating surfaces.
Yet, they are limited by their brittleness, making them liable to crack under high force, and by the difficulties of their manufacture.
These belong to three subclasses, namely, biodegradable, bioactive and inert.
Calcium aluminate and calcium phosphate are examples of the first, being resorbable; hydroxyapatites and glass ceramics, of the second; and alumina, zirconia and carbons, the third.
Where electrical conduction is a priority, inactive metals of the third sort are typically preferred, but biodegradable materials are a better choice when it comes to suture materials. Bioabsorbable materials are used in areas such as vascular stents, intended to provide a long-term but not a permanent framework for repair processes.
Resorbable materials are used in dental and orthopedic procedures (calcium aluminate), as well as for artificial bones, teeth, knees, hips, tendons and ligaments (calcium phosphate).
Bioactive or semi-inert biomaterials like glass ceramics are used to add in bone where required, while hydroxyapatite is used to create bone grafts, fillers and metal implant coatings.
Inert bioceramics such as alumina and zirconia are found in hip and dental implants. Carbon is used to make heart valves and bone scaffolds, and to encourage cartilage regeneration. Silicon nitride is used for spinal fusion implants.

Hip implants can use bioceramics. Image Credit: Monstar Studio/Shutterstock.com
2. Polymers
Natural polymers like starch and collagen are easy to source and break down rapidly, making them suitable for biomaterial use. Synthetic polymers are more commonly useful in making dental and prosthetic materials, implants and single-use medical equipment.
Interestingly, though created for non-medical uses, compounds like polypropylene (PP), polyethylene (PE), polymethylmethacrylate (PMA), polyethylenterephthalate (PEEP), and polyurethane (PU) resemble body tissues in humans so closely in their physical and mechanical qualities that they are now extensively used in biomedicine.
PP is used to create meshes to repair hernias, membranes for extracorporeal membrane oxygenation (ECMO), artificial blood vessel grafts and suture material. Dental implants and bone cements are also constructed with PMA, and vascular grafts from PEEP.
PU is used to make breast implants, wound dressings, patches for heart muscle, and blood vessel grafts, besides drug delivery vehicles. PE is commonly used in making tubes for catheters and drains, hip socket liners and surgical implants.
Polymers are used to make probes that could improve positron emission tomography (PET) imaging. Microelectron mechanical systems (MEMS), better known as lab-on-a-chip, are made of polymer, bringing down the cost of single-use devices.
The adsorptive property of polymers promotes their use as drug-eluting stents (DES). These can be coated with drugs to reduce inflammation, steroids to reduce plaque, or endothelial cells to repair the vessel wall, for instance. Gene-eluting stents are potential developments for the future that could provide a local source of RNA or DNA to inhibit certain genes that cause restenosis.
Polymers lend themselves to the manufacture of inexpensive fibers, films, sheets or synthetic latex. However, their rapid absorption of protein and water makes them liable to contamination outside the body. They are sensitive to heat and chemicals, which complicates their sterilization.
Another disadvantage is their tendency to leach unwanted compounds into the fluids in contact with them. They also tend to break down or wear out. Finally, plastics are already being phased out because of their massive overuse and slow biodegradability.
3. Metals
Metals are often used to make pacemaker wires, vascular stents and implants for the hip and knee joints which require high corrosion resistance and mechanical strength. Both pure metals and alloys are used for such purposes.
The alloys are coated with bioceramics or thin polymer films. Sometimes the surface is engineered for these properties.
These biomaterials are easy to sterilize and to build to specifications, with high shape memory. Conversely, they are cytotoxic in some cases; may cause allergic reactions; and are stiff anddifficult to shape which can hamper osseointegration.
Most metallic biomaterials fall into the following groups: pure titanium or its alloys, stainless steel, and cobalt-chromium alloys.
Titanium alloy is very useful for its lightness, strength and corrosion resistance in human tissues relative to the other two. It is used to make electrode leads, joint prostheses and screws for internal use.
Conversely, titanium wears out faster and may cause osteoarthritis due to its inferior joint surface function. Vanadium is typically found in these alloys and may cause tissue injury over time. It may also, like aluminum, cause neurodegenerative disease such as Alzheimer’s disease (AD).
Stainless steel works well for blood vessel grafts, plates to reunite fractured bones, and guide wires in endoscopic procedures. Cobalt-chromium alloys are used in artificial heart valves, joint prostheses, plates and screws for treating fractures, and teeth.
Hydrogels and other biomaterials
Chitosan and fibrin are instances of natural hydrogels, while polyvinyl alcohol is a synthetic one. These are used to convey therapeutic cargo, including genetic material, proteins or cytokines, in order to treat cancers, autoimmune diseases and inflammatory airway disease.
Micelles are also nanoscale polymers, like hydrogels, used to carry drugs to local lymph nodes. They can carry modified antigens to induce specific cytotoxic immune responses against certain tumors, destroying the cancer cells.
Similarly, polymeric magnetite nanoparticles encasing chemotherapy drugs can pass through the blood-brain barrier (BBB) to treat intracranial tumors.
Liposomes are spherical vesicles composed of phospholipid bilayers, enclosing a therapeutic drug cargo. They were used to encapsulate the messenger ribonucleic acid (mRNA) vaccines from Moderna and Pfizer-BioNTech, that were rolled out to prevent severe coronavirus disease 2019 (COVID-19). Other uses include delivering cancer chemotherapy, antibiotics, analgesics and other pain medication, and hormone therapy, and imaging contrast.
Gold nanoparticles and modified silica nanoparticles are other examples of biomaterials used in chemotherapy, immunotherapy and tumor imaging.

Chitosan is a natural hydrogel found in the outer shell of shellfish. Medicine can be made from it. Image Credit: Sherbak_photo/Shutterstock.com
Biomaterials of human origin
While these biomaterials are extremely useful, they degrade slowly, contributing significantly to medical waste. Newer biomaterials with more rapid biodegradation and increased biocompatibility are being sought to help phase out the older ones and may usher in new therapies and prophylactic strategies.
Newer materials are under study, that use bioactive compounds to achieve specific biological functions. However, at present these are too costly for routine clinical use, or too inconvenient for the patient.
For instance, biomaterials based on the natural extracellular matrix (ECM) provide a biomimetic scaffold. This would allow cells to grow into and infiltrate it to rebuild a strong tissue, ensuring good wound healing. Different ECM components may soon be available for use as required to produce such scaffolds or biomaterials, engineered to achieve the desired mechanical properties.
References
- Brizuela, A. et al. (2019). Influence of the Elastic Modulus on the Osseointegration of Dental Implants. Materials. https://doi.org/10.3390%2Fma12060980. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6472162/. Accessed on July 16, 2022.
- Chong, E. T. J. et al. (2022). Classification and Medical Applications of Biomaterials–A Mini Review. BIO Integration. https://dx.doi.org/10.15212/bioi-2022-0009. https://bio-integration.org/10-15212-bioi-2022-0009/. Accessed on July 16, 2022.
- Chen, F.-M. et al. (2016). Advancing Biomaterials of Human Origin for Tissue Engineering. Progress in Polymer Science. https://doi.org/10.1016/j.progpolymsci.2015.02.004. https://www.sciencedirect.com/science/article/pii/S0079670015000386. Accessed on July 16, 2022.
- Bhat, S. et al. (2013). Biomaterials and Bioengineering Tomorrow’s Healthcare. Biomatter. https://doi.org/10.4161/biom.24717. https://www.tandfonline.com/doi/full/10.4161/biom.24717. Accessed on July 16, 2022.
- Bharadwaj, A. et al. (2021). An Overview on Biomaterials and Its Applications in Medical Science. IOP Conference Series: Materials Science and Engineering. https://iopscience.iop.org/article/10.1088/1757-899X/1116/1/012178. Accessed on July 16, 2022.
Further Reading
Last Updated: Aug 3, 2022