Campylobacter is a genus containing several species of Gram-negative spiral or curved bacteria with one, two or no polar flagellum and a corkscrew motility. They are microaerophilic, but some require hydrogen for growth. They are being recognized as important causes of human gastroenteritis in developed and developing countries and also because of the serious post-infectious sequelae associated with the disease.
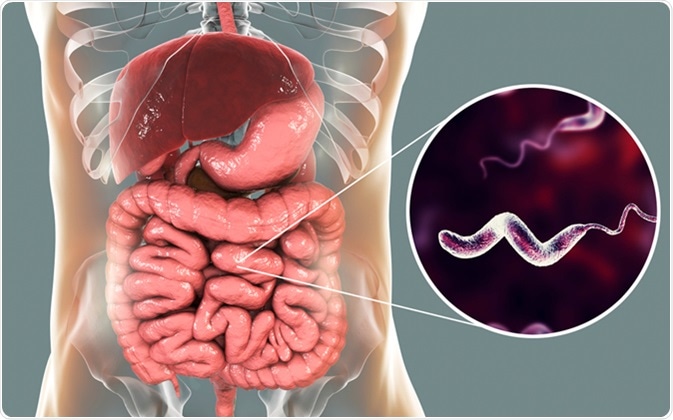
Campylobacter bacteria in intestine, C. jejuni, C. fetus, Gram-negative S-shaped motile bacteria the causative agent of food-borne infection campylobacteriosis, 3D illustration. Image Credit: Kateryna Kon /Shutterstock
Many reliable centers report a rising incidence of gastroenteritis due to Campylobacter infection in the US and the EU. While the reported incidence in the US is about 6 per 100 000 people, unreported cases may number more than 1% of the population with over 100 deaths annually. In the EU, as well, between 2 million and 20 million cases are thought to occur annually within its member states, with a staggering cost in terms of human illness and loss of productivity. In the UK it is thought to have caused 76 deaths in one year (2008) and is now counted as the most frequent cause of food poisoning.
The primary infection of cattle and poultry is from birds, and cross-contamination from infected and undercooked meat and meat products, milk, and drinking water is responsible for the spread of infection. Since Campylobacters are easily inactivated by heating and pasteurization of milk, the proper cooking of animal meat and meat products should bring an end to such sporadic cases or outbreaks. The most common source of identified Campylobacter infection is chicken consumption.
The truth about campylobacter (full version)
Clinical Features
Acute Infection
Infection with C. jejuni or C. coli causes the acute onset of watery or bloody diarrhea, with fever and abdominal cramps. Nausea is common, and vomiting occurs in about 15%. Weight loss is also marked. The incubation period is between 1 and 7 days. Most episodes begin between 24 and 72 hours after ingestion of contaminated meat, but if the amount eaten was small, the onset may be delayed. The symptoms peak at about 24 h to 48 hours. The abdominal cramps may be so sharp as to arouse the suspicion of appendicitis. The episode usually lasts for about a week, on average. The symptoms are due to diffuse enteric inflammation, which later migrates to the colon and the rectum. The intestinal damage may be due to the inflammation or the bacterial toxins. Virulence of the infecting strain is also important in the resulting severity of infection.
In about a third of patients, flu-like symptoms precede the onset of the gastroenteritis, and it has been observed that in such patients the infection is more severe. This may point to some immunologic mechanism of systemic malaise and myalgia resulting from the local enteric infection.
Very young children and young adults are more prone to campylobacteriosis. C. coli is a little more common in adults in their thirties and those who travel to foreign lands, and infections are more likely during the summer months. C. coli accounts for about a fourth of all Campylobacter infections, though C. jejuni is more prevalent. Other vulnerable patient groups include those with hypogammaglobulinemia and AIDS patients, who frequently develop bacteremia and other complications of campylobacteriosis. They also have a 40 times higher incidence of infection with Campylobacter species, and are more likely to have chronic or recurrent infections requiring repeated antibiotic therapy.
On testing, the white blood count is raised, and stool is positive for blood. Campylobacter continues to be excreted in feces for several weeks and this is an important potential point of transmission.
Antibiotics are required only in severe illness, because the gastroenteritis is self-limiting and fluid-electrolyte replacement is all that is necessary in most cases.
Chronic Complications
While the illness typically resolves within a few days, there are significant and varied post-infectious sequelae. These include autoimmune conditions, such as Guillain-Barre syndrome (GBS), Miller-Fisher syndrome, functional gastrointestinal disorders (inflammatory bowel disease, gastroesophageal reflux disorder, and functional dyspepsia), bacteremia and sepsis, periodontal disease and gingivitis, reactive arthritis and meningitis. Their frequency varies from 1 in 1000 for GBS to 7% for reactive arthritis. The health burden of campylobacteriosis is thus large and prolonged.
Further Reading
Last Updated: Feb 26, 2019