Skip to:
Degenerative disc disease is a condition in which the intervertebral discs of the spine become weak and start to deteriorate. There can be a multitude of causes for this condition. Fortunately, there are many treatment options available for degenerative disc disease which vary based on the severity of the disease.
What is degenerative disc disease?
Degenerative disc disease is a medical condition that is characterized by the deterioration of the intervertebral disc in the spine. This results in even further deterioration that affects the facet joints and ligaments surrounding the spine. The condition can affect any region of the spine although it mainly affects the lumbar (L1-L5) and cervical (C3-C7) regions.
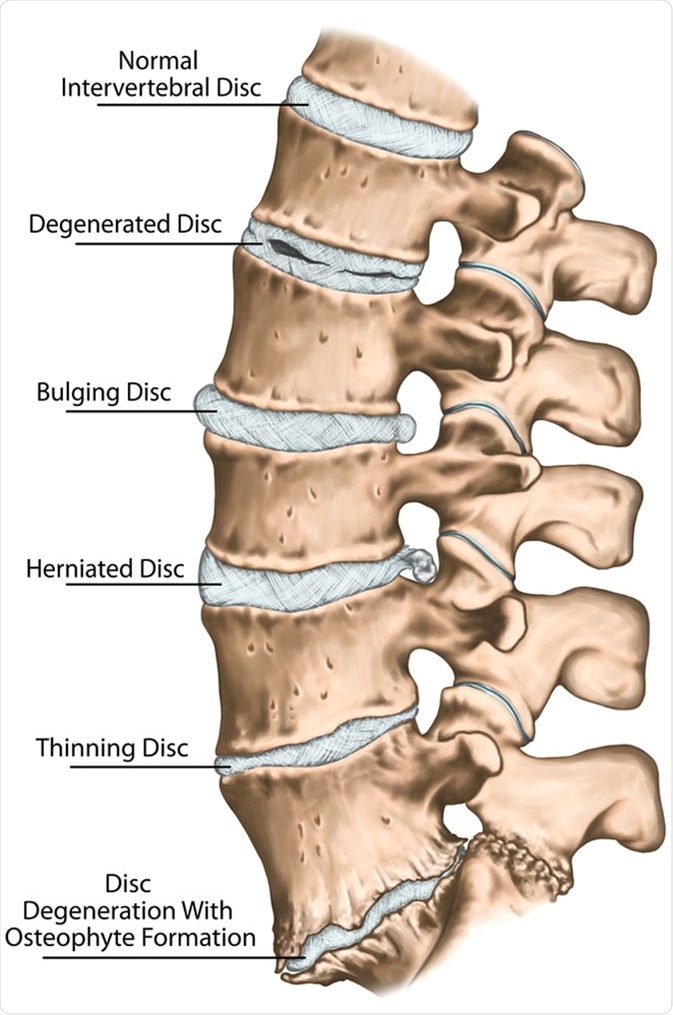
Spine disc problems, degenerative lumbar disc disease, degenerative disc disorder, degenerated disk, bulging disk, herniated disk, thinning disk, disk degeneration with osteophyte formation - Image Credit: Stihii / Shutterstock
The worsening of the discs involves changes in certain properties of the disc, which includes, loss of moisture, reduction in elasticity, and increases in brittleness. The shape of the disc can also be altered which can lead to disc collapse and abnormal spinal movement.
The deformation of the discs can also cause them to bulge towards the spinal canal; potential consequences of this are increased pressure on the nerve roots (radiculopathy) or spinal cord (myelopathy), which leads to various debilitating symptoms.
The main symptoms of degenerative disc disease include general weakness, numbness and tingling of the limbs (paresthesia), chronic pain which is worsened by sitting or certain movements, and loss of balance and coordination.
Degenerative disc disease is very prevalent in older stages of life with approximately 90% of individuals older than 50 years of age having some intervertebral disk degeneration, though it may be asymptomatic. The prevalence is only 40% in persons younger than 30 years of age.
Causes of degenerative disc disease
The main cause of degenerative disc disease is the loss of nucleus pulposus (inner gel-like material) from the center of the disc. This occurs when the outer shell of the disc (annulus fibrosus) is weakened or damaged.
The loss of nucleus pulposus results in a more rigid disc, which in turn increases the pressure on them. This ultimately results in the aforementioned deterioration of all structural elements of the disc within the spinal cord.
Aging, traumatic injuries, and genetic predispositions are the main factors that contribute to this damage.
Additionally, estrogen loss resulting from menopause for women is associated with lumbar disc deterioration; thus, decreased estrogen is considered a risk factor for lumbar disc degeneration.
As degenerative disc disease is a chronic and progressive condition, inflammatory processes are key mediators of the disease and the pain associated with it.
The inflammatory cytokines that contribute to this inflammatory response are tumor necrosis factor (TNF)-α and interleukin (IL)-1β. There is increased production of these inflammatory cytokines by leukocytes and intervertebral disc cells during disc degeneration.
The inflammatory responses caused by TNF-α and IL-1β exacerbate degradation of the extracellular matrix (ECM), further contributing to degenerative disc disease.
The decrease in expression of crucial ECM proteins – aggrecan and collagen – as well as the increase in expression of many proteins that disrupt the ECM – matrix metalloproteinases – are responsible for the collapse of ECM homeostasis.
Treating and preventing degenerative disc disease
Degenerative disc disease cannot be reversed or cured; however, certain lifestyle changes can aid in avoiding further deterioration and help to manage the symptoms.
Many treatments for degenerative disc disease aim to relieve stress and pressure from the spine to aid with the symptoms of the disease.
Chiropractors can loosen the stiffness of the affected vertebra, allowing for the joints to loosen up ad gain ‘nourishment’ through better movement. The spinal readjustment performed by chiropractors can also relax entrapped or compressed nerves providing relief from chronic pain.
Another method of treating cervical degenerative disc disease is cervical artificial disc replacement (C-ADR). This surgical method aims to remove the damaged intervertebral discs then replace it with an artificial disc device.
Preserving the mobility of the spine is the main advantage of this method over other surgical methods, such as fusion.
Reviews around this topic have shown C-ADR to be an effective treatment method for cervical degenerative disc disease; it is both more affordable than more traditional methods and improves the quality of life of patients. Due to the extremely invasive nature of this procedure, it should not be performed for every person with symptomatic cervical degenerative disc disease.
Patients and healthcare professionals must carefully consider when it is appropriate to use this treatment. Additionally, as this treatment option is not widespread the barrier for using this treatment can be the limited availability of this treatment.
Lifestyle changes may also aid in treating the symptoms of degenerative disc disease. Non-weight bearing exercises – hydrotherapies, such as swimming – may help to loosen the spine, relieving pressure from the discs and nerves. Additionally, yoga can stretch spinal muscles allowing the joints to loosen up and become ‘nourished’.
Sources
- Kasbia, V. 2005, Degenerative disc disease: [Final Edition], Pembroke, Ont. https://search.proquest.com/docview/354183403
- Lou, C., et al. (2014). Menopause is associated with lumbar disc degeneration: a review of 4230 intervertebral discs. Climacteric. https://doi.org/10.3109/13697137.2014.933409
- Johnson, Z., et al. (2015). Disc in flames: Roles of TNF-α and IL-1β in intervertebral disc degeneration. European Cells and Materials. https://www.ncbi.nlm.nih.gov/pubmed/26388614
- Pron, G., et al. (2019). Cervical Artificial Disc Replacement Versus Fusion for Cervical Degenerative Disc Disease: A Health Technology Assessment. Ont Health Technol Assess Ser. https://www.ncbi.nlm.nih.gov/pubmed/30847009
Further Reading
Last Updated: Oct 21, 2019