Depression in children is a mood disorder that affects a small, but significant proportion of both young children and adolescents. Up to 8 percent of teenagers and 2 percent of preadolescents are hit by this condition. The term depression ranges over a wide spectrum of mental states, starting from sadness and ending in major depression or bipolar disease (manic-depressive illness).
Risk groups and symptoms
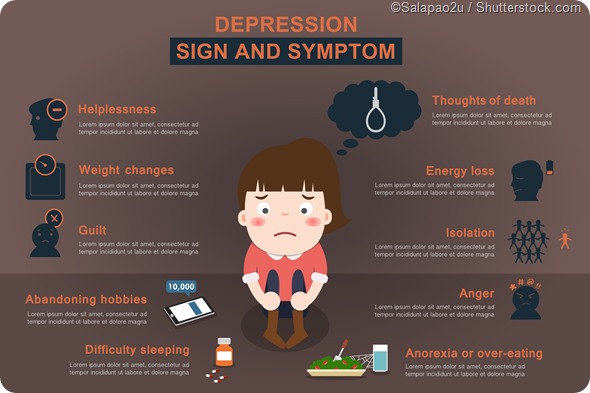
Children at risk for depression share some common factors - namely, a history of depression in the family, and unsatisfactory achievement profile at school. Symptoms that suggest a diagnosis of depression are vague and inconclusive when taken separately, but fit the picture when put together. These include:
- Feelings of hopelessness and emptiness
- Feelings of helplessness and guilt or low self-image
- Loss of interest in previously interesting activities, including loss of interest for school or games
- Low energy or persistent fatigue
- Irritability and quarreling with siblings and friends
- Clinging to the parents in the case of young children
- Bedwetting
- Unrealistic worries such as about a parent’s death
- Insomnia or oversleeping
- Eating disorders or changes in the eating pattern
- Thoughts of suicide and death
- Various physical symptoms – including abdominal pain, headaches and other pains without organic cause and which cannot be successfully treated
All symptoms in this list need not be present for a person to be depressed. Even if the symptoms do not add up to a firm diagnosis, but are significantly present, the person may be suffering from depression and will benefit from appropriate treatment.
Diagnosis
Before a child is diagnosed with depression, it is crucial to perform a full evaluation and rule out any physical causes for the condition. Once organic and physical causes are ruled out, the child should undergo a full interview following a structured pattern, in order to elicit all information of value to the clinician. The symptoms drawn out in that manner should be assessed by using a standardized checklist to meet the criteria for depression.
The symptoms should have been present for at least two weeks to qualify as a depression. Depressed teens may show irritability and negative behavior, apart from misbehaving at school and showing self-pity. It is important to remember that teenagers who have depressive symptoms may also have other disorders such as bulimia or anorexia nervosa, drug addiction or anxiety, apart from physical reasons like pregnancy or induced abortion.
Children who are depressed usually do not know that they should seek help, do not believe they need help or do not think they can be helped. It is for their caregivers to be alert and sensitive to symptoms of depression which do not lift in a few days or weeks, and make sure they are evaluated and treated as necessary.
Childhood Depression
Management
Children and adolescents with mild to moderate depression may be best served by psychotherapy. This can take various forms, such as cognitive-behavioral therapy (CBT), interpersonal therapy (IPT) or problem-solving therapy. These approaches will offer emotional support, support the validity of the child’s feelings, and offer a more hopeful and rational outlook for change.
Medical treatment has been largely confined to tricyclic antidepressants (which have significant side effects) and SSRIs or selective serotonin reuptake inhibitors (which seem to meet with more tolerance). All children should be carefully monitored in view of the high risk of dropping out of school and out of the mainstream, as well as of suicide.
Medical treatment takes time and patience to bear fruit in those patients in whom it is useful. This is because all medications take up to four weeks to show their effects. A series of medicines may be tried before finding the right combination which works for any given individual. It is important not to stop or start these drugs without talking to the healthcare provider first.
If these approaches are unsuccessful, other options such as electroconvulsive treatment (ECT), vagus nerve stimulation (VNS), as well as repetitive transcranial magnetic stimulation (rTMS) may be explored depending on the specific patient profile.
Sources
- http://europepmc.org/abstract/med/11126856
- https://www.nimh.nih.gov/health/topics/depression/index.shtml
- http://www.nimh.nih.gov/health/publications/depression-what-you-need-to-know-12-2015/index.shtml
- http://www.cdc.gov/childrensmentalhealth/depression.html
- http://www.nhs.uk/conditions/stress-anxiety-depression/pages/children-depressed-signs.aspx
Further Reading
Last Updated: Feb 26, 2019