Skip to:
Melanoma, also called malignant melanoma or cutaneous melanoma, is a serious form of skin cancer that develops in the melanocytes. These skin cells produce melanin, which is responsible for skin coloration. If not treated early, melanoma can metastasize to other body parts and become fatal.

Melanoma - a malignant tumor of the skin. Image Credit: Nasekomoe / Shutterstock
What is melanoma?
Melanoma is a tumor caused by uncontrolled growth of melanocytes. One of the major causative factors for melanoma development is DNA damage caused by exposure to ultraviolet (UV) radiation from sunlight or tanning beds/lamps. The most frequent sites of melanoma are those most frequently exposed to UV radiation: the face, neck, trunk (men), and legs (women). Besides skin, melanoma can rarely occur in the eyes, mouth, genital organs, and anal areas.
Melanoma is relative rare, accounting for only 1% of all skin cancers. Because of the high metastatic rate, melanoma is often fatal if not diagnosed and treated at early stages. The lifetime risk of getting melanoma is higher among whites (2.6%) than blacks (0.1%) or Hispanics (0.58%).
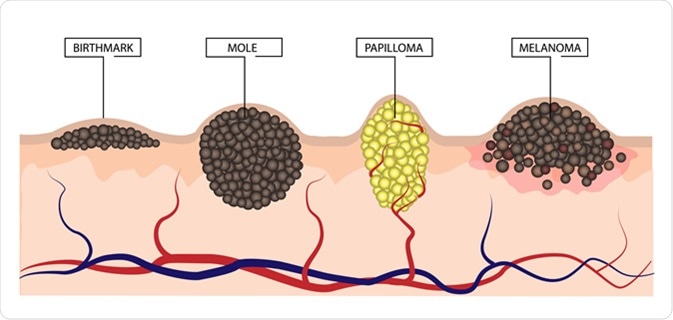
The difference between a birthmark, mole, papilloma and melanoma. Illustration Credit: LiliiaKyrylenko / Shutterstock
How is melanoma diagnosed?
The most prominent early signs of melanoma are altered appearance of an existing mole and/or development of unusual looking new moles on the skin.
To identify unusual moles, it is important to know their basic characteristics. The most prominent features of the moles that may eventually develop into melanoma include:
- Asymmetric or irregular shape
- Irregular border
- Uneven distribution of colors
- Diameter larger than 6 millimeters
- Evolving gradually (changes in shape, size, or color)
These can be remembered as the ABCD signs: Asymmetry, Border, Color, Diameter and any changes in these features.
Skin self-exam, which is done in a well-lit room in front of a full-length mirror, is the best way to examine the skin. A hand-held mirror can be used to check the skin areas that are difficult to see. Doctors generally recommend examining the skin once a month; all skin areas including palms and soles, scalp, ears, nails, and back should be checked thoroughly.
A regular skin examination by a dermatologist is also recommended for people who are at higher risk of melanoma. A dermatologist performs a head-to-toe analysis of the skin using a technique called dermatoscopy, in which they can use a tool to magnify lesions so they are easier to evaluate.

Dermatologist examining for potential melanomas. Image Credit: Africa Studio / Shutterstock
If melanoma is suspected, doctors remove the affected skin area and send it to the laboratory for skin biopsy. Depending on the size and location of the affected area, different types of skin biopsies are available, which are performed under local anesthesia (an injection of pain medicine to numb the area that will be biopsied).
Tangential biopsy is performed when melanoma risk is very low. In this biopsy, the top skin layer is shaved off with the use of a small surgical blade. In technique is not suitable for analyzing deeply invaded melanoma.
Punch biopsy is performed using a tool with a circular blade, which is pressed into the skin around an affected area to remove a round piece of the skin.
Incisional and excisional biopsies are done to detect melanoma in deeper skin layers. Excisional biopsy is performed to remove the entire mole/tumor along with a small portion of surrounding normal skin. In contrast, incisional biopsy is used to remove only the most irregular part of a mole/tumor.
Recently, a novel technique has been developed, which uses reflectance confocal microscopy to directly examine the affected skin area without removing skin tissues.
To check spreading of primary melanoma into nearby lymph nodes, doctors generally recommend performing fine needle aspiration biopsy, surgical lymph node biopsy, or sentinel lymph node biopsy. To determine whether melanoma has spread to other organs (lungs, liver, brain, and spinal cord), various imaging techniques (chest x-ray, CT scan, MRI, and PET) are performed.
How is melanoma treated?
Treatment of melanoma is generally based on cancer stage, size, and location.
For stage 0 melanoma (confined to epidermis), surgery (wide excision) is the best suitable option, which removes the melanoma along with a small portion of surrounding normal skin.
For stage I (thickness: 1 mm) and stage II (thickness: 1 – 4 mm) melanomas, wide excision is performed. In addition, a lymph node dissection is performed if cancer cells are detected on sentinel lymph node biopsy. Doctors sometimes recommend additional therapy with interferon after the dissection.
For stage III melanoma (lymph node metastasis), both wide excision and lymph node dissection are standard treatment strategies. After surgery, additional therapies including immunotherapy or targeted therapy are recommended to reduce the risk of cancer relapse. Targeted therapy is particularly helpful for treating cancer cells with specific genetic mutations. In cases where many lymph nodes are affected, doctors recommend radiotherapy at the site of dissection.
Stage IV melanomas (metastasis to internal organs) are often very difficult to treat. In most cases, both primary tumors and metastases are removed surgically. For non-removable tumors, radiotherapy, chemotherapy, immunotherapy, or targeted therapy is used. Immunotherapy with checkpoint inhibitors, interferon, or interleukin-2 may be effective in treating stage IV melanomas.
Further Reading
Last Updated: Sep 16, 2019