Introduction
Imaging techniques in diagnosing myocarditis
Endomyocardial biopsy and the Dallas criteria
References
Myocarditis represents the inflammatory reaction of the heart due to infectious, autoimmune, or toxic causes. The process can be induced either by exogenous (bacteria, viruses, or parasites) or endogenous (autoimmune diseases and toxins) pathogenic factors. All patients should receive standard heart failure care, while antiviral therapy has limited applicability.
Acute myocarditis (one form of myocarditis) represents one of the most challenging diagnoses in cardiology, as currently, no diagnostic test can be considered a gold standard due to the insensitivity of traditional approaches. Modern techniques have improved the ability to diagnose specific pathogens in the myocardium, increasing interest in inflammatory heart diseases and improving our understanding of myocarditis pathophysiology.

Image Credit: Lightspring/Shutterstock.com
Imaging techniques in diagnosing myocarditis
The initial evaluation of acute myocarditis must encompass detailed medical history and a thorough physical examination, searching for any potential features that may provide clues to its etiology. Additional laboratory and technical examinations should include an electrocardiogram (ECG), serum biomarkers, echocardiography, non-invasive imaging techniques, and endomyocardial biopsy.
Despite its low sensitivity, the electrocardiogram (ECG) is widely used as a screening tool. In acute myocarditis, ECG may reveal sinus tachycardia with non-specific ST-segment and T-wave abnormalities. Atrial or ventricular conduction delay with possible ventricular arrhythmias can also be noted in patients with inflammatory heart disease.
Serum cardiac biomarkers (creatine kinase and troponin) lack specificity but may help confirm myocarditis diagnosis; hence, they are routinely measured in suspected cases. In acute myocarditis, increased cardiac troponin levels are more commonly observed than increased creatine kinase levels. Non-specific serum markers of inflammation (such as C-reactive protein) can also be elevated in myocarditis patients.
Echocardiography represents an important part of the initial diagnostic evaluation when evaluating a patient with myocarditis, assessing the function of the left heart ventricle and ruling out other causes of heart failure (such as valvular, congenital, and amyloid heart disease). Classic findings in myocarditis include global hypokinesis with or without pericardial effusion, although the echocardiographic features are often non-specific.
In recent years cardiovascular magnetic resonance imaging (MRI) has been recognized as a highly sensitive and specific tool for diagnosing myocarditis. This imaging technique has the unique potential to precisely visualize tissue changes, with the prospect of detecting characteristic changes in myocarditis – including interstitial and intracellular edema, hyperemia, capillary leakage, and (in more severe cases) cellular necrosis and ensuing fibrosis.
Contrast-enhanced MRI can also play a significant role in discriminating myocarditis from myocardial infarction, aiding in the evaluation of acute chest pain. In myocarditis, the infiltrates are usually located in the mid-wall and tend to spare subendocardial tissue, whereas the subendocardium is involved first in infarction. New contrast techniques using segmented inversion recovery gradient-echo pulse sequences and gadolinium enhancement can distinguish between diseased and normal myocardium even better.
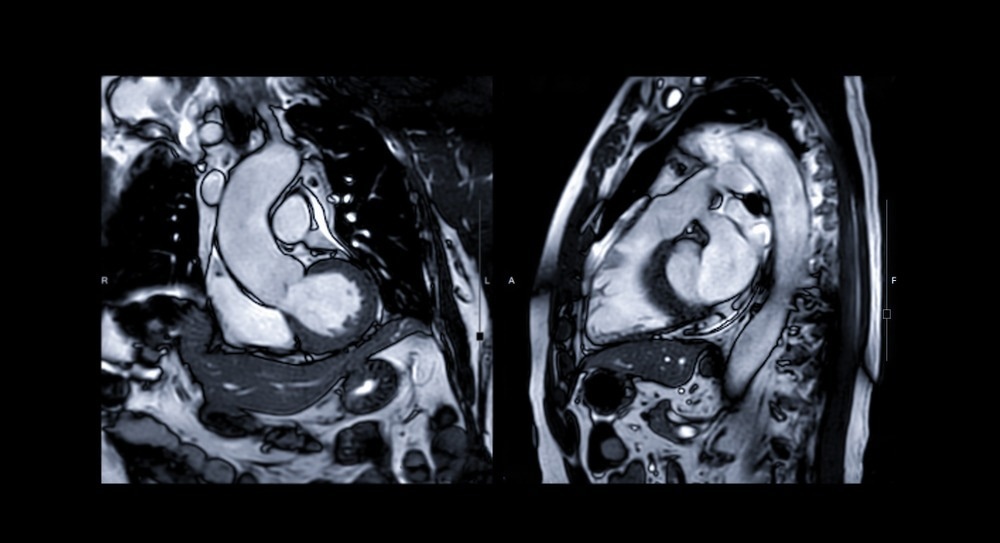
Image Credit: Radiological imaging/Shutterstock.com
Endomyocardial biopsy and the Dallas criteria
Histologic examination of heart tissue is necessary to confirm the diagnosis of myocarditis; thus, endomyocardial biopsy still represents one of the key diagnostic steps. Nevertheless, the applicability of endomyocardial biopsy is often hampered by sampling errors from patchy inflammatory infiltrates and inconsistency in observer interpretation.
The standard Dallas pathological criteria, published in 1986, served as the initial attempt to develop standardized diagnostic guidelines for the histopathological classification of myocarditis. The presence of an inflammatory infiltrate with or without necrosis under a light microscope was required for the histological diagnosis of myocarditis, but sampling error, low sensitivity, and lack of prognostic value hindered the further use of these criteria.
Therefore, immunohistochemistry which allows quantification, identification, and differentiation of inflammatory cells (using monoclonal antibodies), is gaining further acceptance in diagnosing myocarditis. The main criterion for immunohistological diagnosis of inflammatory cardiomyopathy is specified quantitatively as more than 14 infiltrating leukocytes per mm2 (preferably T-lymphocytes or activated T-cells).
References:
- Magnani, J.W. and Dec, G.W. (2006). Myocarditis. Circulation, 113(6), pp.876–890. doi:10.1161/circulationaha.105.584532.
- Cooper, L.T. (2009). Myocarditis. New England Journal of Medicine, [online] 360(15), pp.1526–1538. doi:10.1056/nejmra0800028.
- Kindermann I, Barth C, Mahfoud F, et al. Update on Myocarditis. J Am Coll Cardiol. 2012 Feb, 59 (9) 779–792.https://doi.org/10.1016/j.jacc.2011.09.074
- Robert Dennert, Harry J. Crijns, Stephane Heymans, Acute viral myocarditis, European Heart Journal, Volume 29, Issue 17, September 2008, Pages 2073–2082, https://doi.org/10.1093/eurheartj/ehn296
- medlineplus.gov. (n.d.). Myocarditis: MedlinePlus Medical Encyclopedia. [online] Available at: https://medlineplus.gov/ency/article/000149.htm.
- Andréoletti, L., Lévêque, N., Boulagnon, C., Brasselet, C. and Fornes, P. (2009). Viral causes of human myocarditis. Archives of Cardiovascular Diseases, 102(6-7), pp.559–568. doi:10.1016/j.acvd.2009.04.010.
Further Reading
Last Updated: Sep 11, 2023