The Middle East respiratory syndrome coronavirus (MERS-CoV) is a respiratory virus that was first reported in Saudi Arabia in 2012.
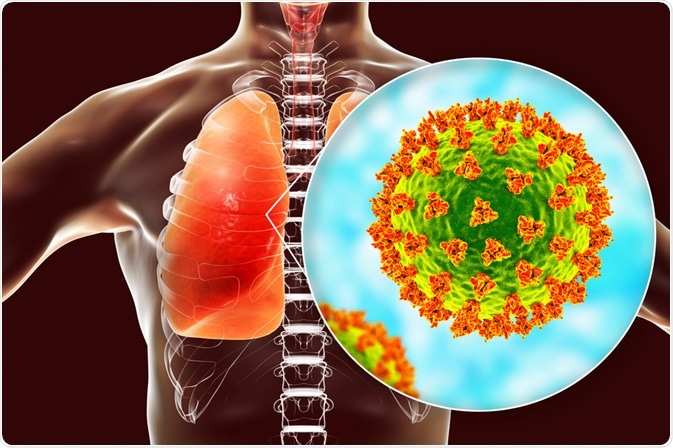
Image Credit: Kateryna Kon / Shutterstock.com
From Saudi Arabia, MERS-CoV traveled to other countries, most of which included nations within the Arabian Peninsula including Qatar, Oman, Jordan, Kuwait, Yemen, Lebanon and the United Arab Emirates. Since the outbreak emerged, over 2,000 MERS-CoV cases have been reported, of which 800 individuals succumbed to the virus.
MERS-CoV is a type of human coronavirus known as a betacoronavirus. Although the precise source of MERS-CoV has not been confirmed, it is believed to have originated from bats, with dromedary camels serving as the intermediate hosts until the infection originally reached humans.
Drug targets of MERS-CoV
Like many other coronaviruses, the MERS-CoV consists of four structural proteins known as the spike (S) protein, envelope (E) protein, membrane (M) protein and the nucleocapsid (N) protein. In addition to these proteins that are typically found in most coronaviruses, MERS-CoV also contains two large polyproteins known as pp1a and pp1ab. Taken together, both the structural and non-structural proteins that make up the MERS-CoV have been used as therapeutic targets.
Treatment options
The four primary approaches by which MERS-CoV can be treated include the repurposing of existing clinically approved drugs, convalescent plasma (CP) and whole blood therapy, intravenous administration of immunoglobulin (IgG) and monoclonal antibodies (mAbs). In addition to these, several other therapeutic agents have been assessed for their efficacy in treating MERS-CoV.
Repurposing drugs
By definition, the repurposing of existing drugs that have been clinically approved by the United States Food and Drug Administration (FDA) allows for existing drug molecules to be used to treat new diseases. Through the use of high throughput screening technologies, researchers can evaluate large libraries of drug compounds and small molecules for their potential activity against novel targets. Not only does the repurposing of drugs save time when novel diseases arise and need to be treated immediately, but it also reduces the costs associated with developing an entirely new drug.
Several different drugs have been evaluated for their antiviral activity against MERS-CoV, including:
- Ribvarin
- Hexachloropene
- Nitazoxanide
- Homoharringtonine
- Ayoclovir
- Chloropromazine hydrochloride
- Trifluopromazine hydrochloride
- Imatinib mesylate
- Dasatinib
- Chloroquine
- Loperamide
- Lopinavir
CP and whole blood therapy
CP therapy involves the use of whole blood or plasma that has been collected from patients who have recently recovered from the viral disease of interest. During the MERS-CoV epidemic, the administration of CP and other neutralizing antibodies were particularly useful, as no specific vaccine or drugs were available for treating this disease.
Despite the utility of this treatment approach, the lack of eligible donors who were both previously infected with MERS-CoV and had sufficient levels of antibodies were scarce. Furthermore, there is a lack of evidence that definitively proves the efficacy and safety of CP and whole blood therapy in the treatment of MERS-CoV.
Intravenous Ig
Ig products that are used for the intravenous treatment of MERS-CoV patients are obtained from serum products that were originally intended for autoimmune and inflammatory disease therapies. Several different health conditions that have benefited from the administration of intravenous Ig (IVIG) include heart failure, mycobacterial infection, epilepsy, and Alzheimer’s disease.
To date, there is no evidence that supports the anti-MERS activity of IVIG. Furthermore, the chance that an IVIG treatment can cause renal failure or thrombosis in MERS patients is high, thereby limiting its clinical use.
Therapeutic antibodies
Both mAbs and polyclonal antibodies have been evaluated for their antiviral activity against MERS-CoV. In fact, severe MERS-CoV infection can be treated with the LCA60 antibody, which was originally derived from the B cells obtained from a human donor who was recovering from MERS.
Preclinical studies have found that both mAbs and polyclonal antibodies that have been specifically targeted against the cellular receptor dipeptidyl peptidase 4 (DPP4) successfully inhibit MERS-CoV in vitro. Comparatively, two mAbs known as MERS-4 and MERS-27 have shown strong neutralizing activity against MERS-CoV as a result of their inhibitory action in the receptor-binding domain of the MERS-CoV S protein. Another study found that two novel antibodies known as REGN3051 and REGN3048 are effective in treating MERS-CoV in animal models.
Prevention and control

Image Credit: Drazen Zigic / Shutterstock.com
Due to the known risk of transmission within hospitals and healthcare systems in general, contact isolation, droplet isolation, and airborne infection control precautions should be instituted, particularly during aerosol-generating procedures. Until the transfer, all patients should wear a face mask and should be isolated in a closed-door room. Additionally, hand hygiene should be strictly performed and all visits to the sick patient should be controlled and restricted.
At the moment, there is no licensed vaccine for MERS-CoV. Therefore, its development has been the focus of many different research laboratories. Vaccination of dromedary camels is one way to reduce zoonotic transmission, although the long-term effects of such a strategy remain to be seen.
References
- Mustafa, S., Balkhy, H., & Gabere, M. N. (2018). Current treatment options and the role of peptides as potential therapeutic components for Middle East Respiratory Syndrome (MERS): A review. Journal of Infection and Public Health 11(1); 9-17. doi:10.1016/j.jiph.2017.08.009.
- Sutton, N. R., & Kawamoto, K. R. (2021). Lessons Learned from the MERS-CoV Outbreak. Cardiovascular Revascularization Medicine 24; 24-25. doi:10.1016/j.carrev.2020.12.007.
- Al-Dorzi HM, Van Kerkhove MD, Peiris JSM, Arabi YA. Middle East respiratory syndrome coronavirus. In: Hui DS, Rossi GA, Johnston SL. SARS, MERS and other Viral Lung Infections: ERS Monograph 72. European Respiratory Society, 2016; pp. 21-34.
- Al-Tawfiq JA, Memish ZA. The Middle East Respiratory Syndrome Coronavirus Respiratory Infection: An Emerging Infection from the Arabian Peninsula. In: Kon K, Rai M, editors. The Microbiology of Respiratory System Infections. Academic Press, 2016; pp. 55-63.
Further Reading
Last Updated: Mar 21, 2021