Natural family planning (NFP) is a method of contraception which depends upon increasing a couple’s awareness of a woman’s fertile days, until they are able to plan to achieve or avoid pregnancy as they desire. It involves training in recognition of various physical changes that indicate the onset of the fertile period.
The 28-day menstrual cycle includes about six days of fertility – days on which an oocyte is available for fertilization by a sperm. These start five days before ovulation and extend to the day of ovulation itself. The exact timing of ovulation is monitored by various indicators, and therefore, this training may take longer in women with irregular cycles, but is still very much possible.
How effective is it?
Various NFP methods have been estimated to have a 99 per cent efficacy, but this figure may not take into account the fact that many couples may take a risk even if they are not sure the woman is infertile. Thus a more realistic figure would probably be 75 per cent with typical use.
The lowest failure rate is achieved by the use of multiple indicators, and when they are used for each cycle. Sometimes combined NFP is used, which means that condoms or other barrier methods are also adopted during the days of the cycle when fertility is high. It is important to note that sole practice of NFP will not offer protection against STIs.
Methods
Various methods are used to achieve NFP, including:
- Standard days based on the length of the menstrual cycle, based on charting six to twelve cycles can be used to predict when ovulation will occur in future cycles. It is not reliable during periods of amenorrhea, such as the postpartum, or when cycles are very irregular, such as in the perimenopause or lactation.
- Cervical mucus characteristics - these change from clear and copious on fertile days, to a peak volume on the day of ovulation, to thick and opaque in the second half of the cycle.
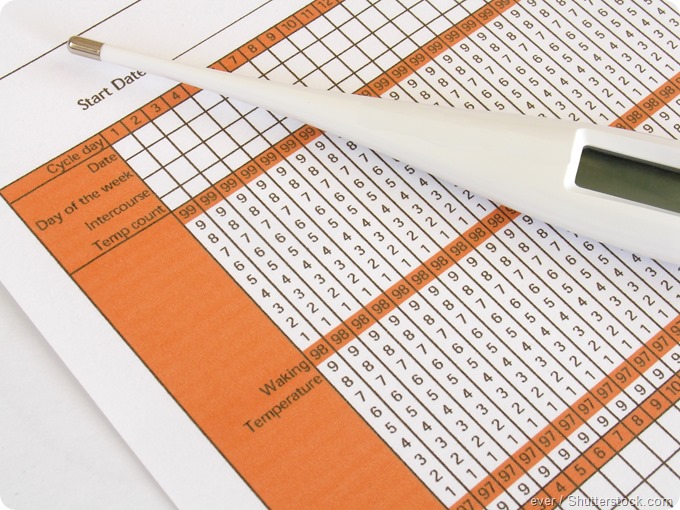
- Basal body temperature (BBT) is based on measurement of the temperature every morning as soon as the woman wakes, before she does anything else. It usually registers a dip which precedes ovulation by 12-24 hours. It then goes up slightly and remains there for the second half of the cycle.
- The symptothermal method combines the woman’s observation of all the above physical changes rather than one alone, along with others such as mittelschmerz (ovulation pain).
- Coitus interruptus, or the withdrawal method, consists of the male partner removing the penis from the vagina just before ejaculation. It has obvious disadvantages such as the interruption of the act of intercourse, and is unreliable since the sperm ejaculated just outside the vagina can still swim inside and cause pregnancy. Pre-ejaculation fluid also contains viable sperm in many cases. It has the highest risk of pregnancy among NFP methods.
- Lactational amenorrhea method (LAM) is an age-old method. Breast feeding acts to reduce the frequency of ovulation by increasing the levels of prolactin, a pituitary hormone, which suppresses gonadotropin activity. The LAM is suitable for women who are lactating under the following conditions:
- Within six months of childbirth
- Complete amenorrhea persists
- Exclusive breastfeeding is performed
The efficacy is about 0.5 percent in such situations. However, some women do become pregnant before they have their first postpartum periods, because ovulation occurs two weeks prior to menstruation. After six months, therefore, it is better to use backup methods in addition to LAM.
Conclusion
NFP has many advantages, such as increasing a couple’s interaction and confidence in sexual relationship, religious acceptability, and low cost, besides the absence of any other medication or device. It helps a woman become more aware of her own body and fertility as well, however its practice may be more difficult following abortion or miscarriage, during a postpartum or breastfeeding phase, or following the halt of hormonal contraception as well for those who experience persistently irregular periods.
NFP also comes with disadvantages such as no protection against STIs, required abstinence or use of alternative contraception during fertile period and careful, daily record keeping of fertility signs. Illness, hormonal treatments, stress, travel and lifestyle factors can disrupt fertility signs and contraception effectiveness can vary greatly depending on the accuracy of NFP implementation.
References
- https://www.hhs.gov/opa/pregnancy-prevention/non-hormonal-methods/natural-family-planning/index.html
- http://www.fpa.org.uk
- https://www.ncbi.nlm.nih.gov/pubmed/1596436
- http://healthywa.wa.gov.au/Articles/F_I/Fertility-awareness-natural-family-planning
- http://www.nhs.uk/Conditions/contraception-guide/Pages/natural-family-planning.aspx
Further Reading
Last Updated: Dec 29, 2022