A suspected case of rabies should be treated as soon as possible, even if there are not any signs or symptoms of the disease yet.
Shortly after suspected exposure to the rabies virus, patients should be vaccinated prophylactically to prevent the virus from infecting the individual.
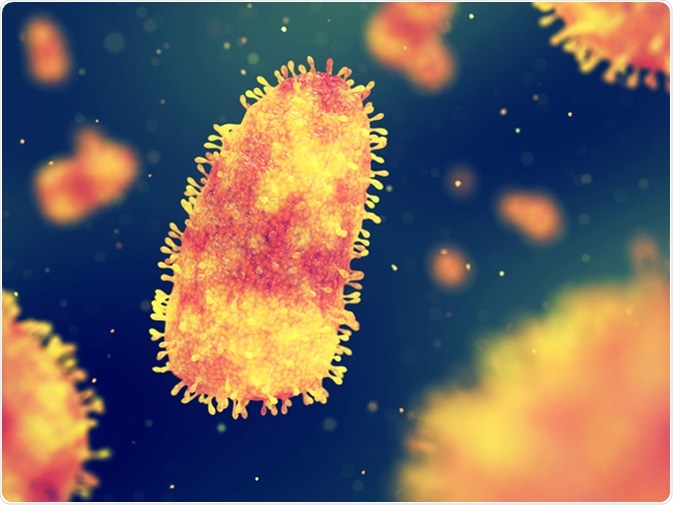
Rabies is a deadly viral disease of the nervous system, Rabies virus infection, 3d illustration. Image Credit: nobeastsofierce / Shutterstock
There is currently no known cure for the disease if the patient is already experiencing symptoms. Therefore, the aim of treatment for a symptomatic patient is to prolong his/her lifespan and keep the individual as comfortable as possible.
These two treatments, depending on the progression of the disease, clearly differ significantly and are covered in more detail below.
Post-Exposure Prophylactic Treatment
Exposure to the rabies virus most commonly occurs following a bite from an animal that is infected.
Shortly after the incident, it is important to perform post-exposure prophylaxis (PEP) treatment to prevent the virus from infecting the patient and causing the disease to progress.
There are three major categories of contact with the suspected rabid animal that warrants different PEP treatments.
These include:
- Category I: Involves touching or feeding animals, licks on intact skin
- Category II: Involves the rabid animal nibbling uncovered skin that results in minor scratches or abrasions without any visible bleeding
- Immediate vaccination
- Local wound treatment
- Category III: Involves a single or multiple bites or scratches that break the skin (transdermal wounds), licks on broken skin, saliva contamination with the mucous membrane from licks or any contact with bats.
- Immediate vaccination
- Administration of human rabies immunoglobulin (HRIG)
- Lock wound treatment1
Category II and II cases both involve immediate local wound treatment, of which involves a thorough flushing and washing of the wound for a minimum of 15 minutes with the following substances:
- Soap and water
- Detergent
- Antiseptics
- Povidone iodine
- Alcohol
- Iodine tincture
Once the wound has been cleaned thoroughly, a simple dressing without the use of stitches should be applied.
Avoiding stitches when dressing the wound is important, as stiches increase the likelihood of the virus entering the nervous system and infecting the rest of the body.
It is important to note that the rabies virus to be transmitted in other ways, such as from animal saliva entering the eye of an individual. If this occurs, the eye should be washed thoroughly with water and the rest of the process should continue to be followed as previously stated.
In addition to wound treatment, both Category II and III cases require a health professional to immediately administer the rabies vaccine, whereas Category III requires timely injections of HRIG.
The difference between the rabies vaccine in HRIG involves the rate at which immunity from the rabies virus occurs.
A course of rabies vaccines that are injected into the shoulder muscle provide affected individuals with long-term immunity; however, this effect may take several days to occur.
As a result, HRIG is typically administered directly to the wound or site of injury to provide immediate protection against the rabies virus while the vaccine injections are given more time to develop.
HRIG is a preparation of antibodies that help to prevent the rabies virus from reaching your nervous system. By providing an immediate effect to neutralize the virus and inhibit spread throughout the human body. Whilst it may cause some irritation at the site of the action, it has a good side effect profile in most cases.
Note that individuals who have been previously vaccinated against rabies will not typically require HRIG treatment.
However, regardless of whether the patient has been previously vaccinated against rabies, every patient that is suspected to have come into contact with the rabies virus should be given a course of rabies vaccine treatments as a precautionary method.
Patients who have been previously are only required to be vaccinated two of the typical four vaccination treatments.
In the standard case, four injections are administered in the muscle of the upper arm on:
- Day 1 of treatment
- Day 3 of treatment
- Day 7 of treatment
- Day 14 of treatment
- * a fifth injection on Day 30 of treatment is required for individuals with a weakened immune system
Some patients may notice redness, swelling or pain at the site of injection, usually a day or two after administration.
Symptomatic Treatment
If the rabies virus has been transmitted to someone and appropriate medical attention was not sought in a timely manner, the individual may experience symptoms such as hyperactivity and fear of water or air.
Unfortunately, at this point in time there is no known cure for rabies that has established to the point that these symptoms arise. As result, symptomatic treatment has a strong focus on increasing quality of life by keeping patients comfortable.
Tranquilizers and sedatives are often used to minimize physical pain, as well as the emotional turmoil a diagnosis with rabies can present.
References
Last Updated: Jul 14, 2023