The neural processes involved in the pathophysiology of schizophrenia are not well understood, and there are several mechanisms that are thought to play a role.
Several neural transmitters appear to be involved, particularly dopamine and glutamate. However, there are also other theories that consider dysfunction of interneurons, the immune system and oxidative stress.
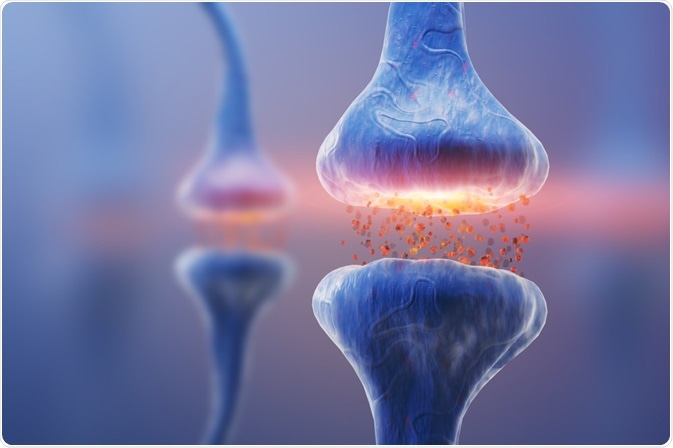 Image Credit: KateStudio / Shutterstock.com
Image Credit: KateStudio / Shutterstock.com
Dopamine hypothesis of schizophrenia
The dopamine hypothesis originated from the observation that many antipsychotic medications that helped to reduce the symptoms of schizophrenia, such as phenothiazines, had an antagonistic effect on the dopamine neurotransmitter.
This led to the idea that dopamine plays a role in the pathophysiology of schizophrenia and was supported by further research showing that drugs with an agonist effect on dopamine, such as amphetamines, aggravate the psychotic symptoms associated with schizophrenia.
Dopamine is thought to be linked to the positive symptoms of schizophrenia and has a less profound effect on negative symptoms. It is for this reason that traditional psychotic medications, which acted on the dopamine neurotransmitter, were more effective on positive symptoms.
However, in addition to dopamine, it is likely that another neurotransmitter, serotonin, is also involved in the pathophysiology. This is because emerging research has indicated that newer generation atypical antipsychotic medications also have a similar effect on the positive symptoms of schizophrenia, although their mechanism of action involves serotonin.
Glutamate hypothesis of schizophrenia
The neurotransmitter glutamate and the NMDA glutamate receptor are also thought to be involved in the neural processes of the brain that may lead to schizophrenia.
In particular, low levels of glutamate receptors have been associated with patients who are affected by schizophrenia, suggesting a link between the two factors. To further this idea, medications that antagonize the glutamate receptor neural pathway, such as phencyclidine and ketamine, have been shown to mimic the cognitive symptoms of schizophrenia.
However, it appears the glutamate has a more profound effect on the negative symptoms of schizophrenia, rather than the positive symptoms. For this reason, positive symptoms do not respond well to medication that targets the glutamate neural pathways.
Kynurenic acid
Kynurenic acid is an amino acid that may be involved in the neural pathways of schizophrenia, as it has been observed in higher concentration than normal in affected patients.
This is thought to be due to the action of the acid as an NMDA receptor antagonist and resulting decrease in glutamate activity. As it is closely linked to the glutamate pathway, it is primarily involved with the negative symptoms associated with the condition.
What is schizophrenia? - Anees Bahji
Interneuron dysfunction
Interneurons in the brain may also be involved in the pathways of schizophrenia, due to their GABAergic action.
This emerging concept was originally suggested due to the observation that patients with schizophrenia were likely to have decreased levels of a particular protein in a small subset of cortical neurons. The interneurons were also associated with the expression of parvalbumin protein, which is thought to be involved with the neural pathways of the disease.
Oxidative stress
More recently, researchers have taken an interest in the role of oxidative stress in the neural pathways of schizophrenia.
Unregulated reduction and oxidation reactions in early development may affect certain cells and lead to susceptibility to the disease. It is now yet clear how this affects the brain cells involved, such as oligodendrocytes, but it has been suggested it may be linked to abnormalities in the white matter.
References
Further Reading
Last Updated: Feb 10, 2021