The current standard of care for diabetes
Targeting the cause: therapies aimed at pancreatic cell regeneration
Immunotherapy in the works for diabetes
Dietary supplements for diabetes treatment
Microbiome-based therapies for diabetes in the pipeline
Protein inhibitors for type 2 diabetes
Hormone-based therapies
References
Further reading
Diabetes is a metabolic disorder characterized by a deficiency in the hormone insulin, insulin resistance, or both.

Image Credit: Buravleva stock/Shutterstock.com
Generally, there are several subtypes of diabetes. However, the two most prevalent are type 1 and type 2. Type 1 diabetes is an autoimmune disease that results from the autoimmune destruction of the pancreatic beta cells, which produce insulin. In patients with type 2 diabetes, cells are resistant to the action of insulin, a phenomenon caused as a result of obesity and deficient incident secretion.
Insulin is essential in metabolism, preventing hyperglycaemic emergencies (dangerous elevation in blood sugar levels which is considered a metabolic emergency), but also is necessary to prevent long-term complications of diabetes by swiftly correcting both fasting and postprandial (after consumption) hyperglycemia. Ultimately, glucose control is critical to achieving positive long-term outcomes, as the complications of both ongoing and persistent hyperglycemia lead to several comorbid states. These include retinopathy, neuropathy, nephropathy, and cardiomyopathy.
Diabetes is a complex disease and subsequently requires a multifaceted approach to treatment. Evidence suggests that lifestyle interventions are particularly influential in the development and further complications associated with type 2 diabetes in susceptible populations. However, to prevent the high risk of subsequent complication development, treatment with several types of medication alongside permanent life changes is often required in diabetes.
The current standard of care for diabetes
Despite the successful development of several new therapies for the treatment of type 2 diabetes, such as Glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose cotransporter-2 inhibitors, there is a continued effort to discover novel treatment options that can provide more efficacious glycemic control with reduced risk of complications/ improved safety.
Insulin is considered the most transformative discovery in medicine. It was first isolated in 1921 and allowed type one diabetes to be a treatable rather than terminal illness. However, one hundred years after its discovery, insulin is becoming increasingly obsolete. Despite advances in automated incident delivery systems, individuals must exert conscientious efforts to manage their physiology. Despite the treatable nature of diabetes, the life expectancy of a person with type one diabetes is 12 years below average.
As such, the current paradigm of type 2 diabetes prevention and treatment is shifting, with many therapies targeting various aspects of the disease pathology emerging – and many are curative.
Targeting the cause: therapies aimed at pancreatic cell regeneration
Increasingly, a cure for type 1 diabetes has come into focus; this curative outlook is focused on replacing the beta cells rather than supplying the body with insulin.
The first reported evidence of meal-regulated insulin secretion by differentiated stem cells earlier in 2021 with interim results from a multicentre clinical trial period the implants of 20 patients consist of pancreatic endoderm cells derived from human pluripotent stem cells; the safety, tolerability, and efficacy of the implants were tested in 26 patients in phase I/II trial.
Despite the absence of relevant clinical outcomes, the study demonstrates an important milestone, demonstrating the ability of pancreatic endoderm cells (PECs) to mature into glucose-responsive, insulin-producing mature beta cells in vivo in patients with type 1 diabetes.
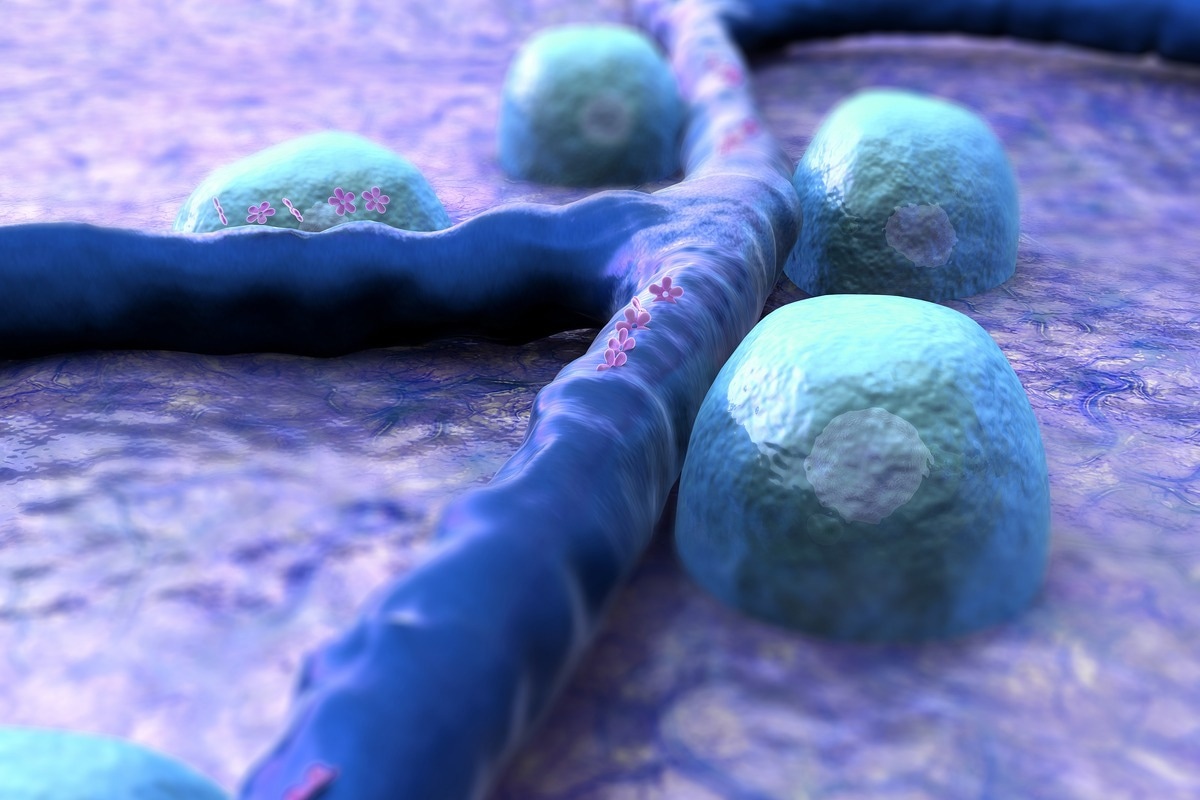
Image Credit: UGREEN 3S/Shutterstock.com
These early-stage findings support future investigations into optimizing cell therapies for diabetes.
Immunotherapy in the works for diabetes
Another curative approach to type 1 diabetes is strategies for suppressing or evading the immune system. This is because type 1 diabetes is caused by a disproportionate autoreactive response of the immune system that can no longer tolerate itself. An organism's ability to self-tolerate depends on the balance between central, peripheral, and organ-specific immune regulation. A disruption to this homeostasis results in auto-reactivity.
Antigen-specific immunotherapy is the administration of autoantigens, which, in the context of type 1 diabetes, involves islet-antigen-specific tolerization of CD4+ and CD8+ T cells. This can be achieved through several tolerogenic mechanisms, the most prevalent of which is the restoration of regulatory T cells, effector T-cells, etc.
Tolerization refers to the tolerance of the immune system to a particular antigen. In the context of diabetes, the antigen is on the surface of the beta cells. The ways that this can be achieved are multifaceted, with immunotherapies working differently.
Some immunotherapies are centered on targeting the B cells, while others ameliorate the activities of both B-cells and killer T cells, so they cannot induce that destructive effects. Some treatments may also augment the effect of regulatory T cells to prevent pancreatic auto-reactivity.
How There Could Finally Be A Cure For Diabetes
Dietary supplements for diabetes treatment
A French biotech company, Valbiotis, has developed a dietary supplement comprising a combination of extracts from five plants. In July 2019, they announced positive results from a phase IIA study of their compound which sought to evaluate its efficacy in pre-diabetic populations compared to placebo.
Microbiome-based therapies for diabetes in the pipeline
In 2019, positive results from a phase 2 study of a microbiota-based dietary supplement were published. Eubacterium hallii, considered a next-generation probiotic, is being studied in a double-blind, run demised, placebo-controlled trial to assess its safety and efficacy with 12- week supplementation. This comes after increased evidence of the role of bacteria, which form a large percentage of the gut microbiome, in human health and disease. Previous studies have highlighted the therapeutic potential of these specific bacteria in preventing and treating gastrointestinal, metabolic, and other diseases.
Protein inhibitors for type 2 diabetes
Apabetalone (RVX-208) is a small molecule inhibitor of bromodomain and extra-terminal (BET) proteins. This is a histone acetylation reader that is responsible for causing pro-inflammatory and pro- atherosclerotic gene transcription.
Once they are bound to chromatin, BETs can recruit chromatin remodeling and transcription elongation factors which allow transcription via RNA polymerase. As they play a vital role in the transcription of cytokine response genes implicated in inflammation, vascular function, and lipid metabolism, inhibiting their activity could help treat chronic inflammatory and metabolic diseases such as diabetes. This treatment has completed phase II clinical trials in pre-diabetic models.
Hormone-based therapies
For those currently diagnosed with type 2 diabetes, a pharmaceutical drug that can activate the production of hepatic insulin-sensitizing substance (HISS) is in the pipeline. This hormone is known as hepatalin. In the absence of adequate insulin, hepatalin stimulates the body's ability to partition glucose into the muscle.
The future of diabetes treatment is evolving, with new treatment paradigms targeting various aspects of the pathological causes of both type one and type 2 diabetes. Currently regarded as an epidemic by the World Health Organization, with an estimated 700 million individuals predicted to be affected by 2045, there currently remains an unmet need. As such, the global diabetes drug market is projected to reach 68 billion by 2026, prompting the emergence of revolutionary technologies and pharmaceuticals to cure or significantly improve the efficacy of currently available standard-of-care, traditional insulin-based treatment.
References
Further Reading
Last Updated: Jun 29, 2022