Vertebroplasty denotes a shorter term for percutaneous vertebroplasty, which is an image-guided therapeutic approach used for the treatment of painful or unstable vertebral body compression fractures that are unresponsive to conservative therapy.
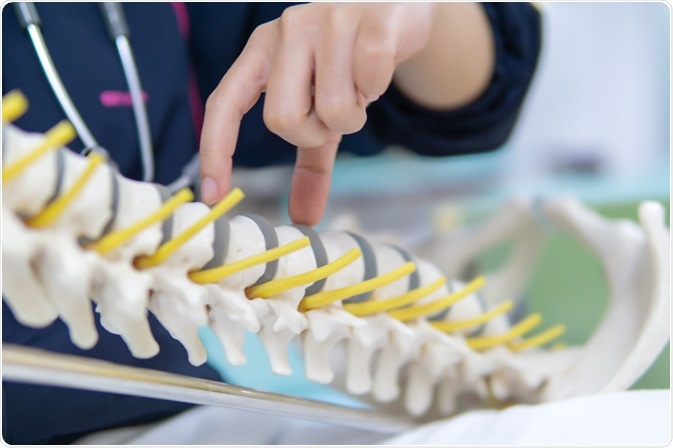
Image Credit: nuiza11 / Shutterstock.com
What is a vertebroplasty?
In this procedure, a trocar is placed into a fractured vertebral body, followed by the application of an acrylic polymer that provides bone augmentation and prevents further collapse of the vertebrae.
Before vertebroplasty was introduced, vertebral compression fractures were essentially the only type of fractures not treated orthopedically. These injuries were treated conservatively, relying on bed rest and the administration of analgesics – neither of which are completely benign and without any adverse effects.
The principal aim of vertebroplasty is to alleviate pain and improve mobility of the patient, while vertebral body stabilization is considered a secondary goal. Thus, this treatment modality is directed towards affected individuals, particularly elderly patients, who had a reasonable course of medical therapy but are still suffering pain.
Technical aspects of vertebroplasty
Vertebroplasty is typically performed on an outpatient basis; therefore, important pre-procedure instructions should be provided to the patient at the time of the evaluation. This method of treatment should be avoided in individuals with known infections and fevers, as well as in those with elevated white blood cell (WBC) counts. General anesthesia is usually not administered; however, it can be an option when dealing with uncooperative patients or patients who are in extreme pain.
Different vertebroplasty techniques emerged based upon predominantly North American and European experiences, although variations between them are mostly minor and related to the availability of equipment and products utilized, as well as the operator’s training and personal style.
Vertebroplasty & Kyphoplasty ( Spine Surgery) Neuro Surgery; Fortis Healthcare,India
Needle placement within the vertebral body is typically guided either by standard fluoroscopy, computed tomography (CT)-guidance, or CT fluoroscopy. Regardless of the modality used to position the needle, acrylic injections are a form of venous embolization; therefore, these injections should always be performed under continuous, high-quality fluoroscopic observation.
Vertebroplasty can restore vertebral height in cases of fragment instability with intravertebral clefts, which indicates non-union of the fracture fragments. Vertebroplasty of the thoracic and lumbar spine is commonly performed by a transpedicular or parapedicular approach, with patients in the prone position.
A myriad of bone cement types is commercially available, although they vary in terms of cost, polymerization rate, radio-opacity, and biocompatibility. Polymethylmethacrylate is the most frequently used bone cement for vertebroplasty. The end goal of this procedure is to deliver the cement evenly in the vertebral body in order to stabilize the fractured vertebra by increasing its mechanical strength. It is crucial during the cement injection to avoid extra-vertebral cement delivery.
Postprocedural course
In an outpatient setting, the majority of patients who undergo vertebroplasty are observed for only two hours before being discharged. Individuals remain in the supine position for one hour and are gradually allowed to sit up or stand over the next hour under the direct supervision of a physician or a nurse.
Most patients experience immediate pain relief, which can be a result of thermal necrosis and chemotoxicity of the intraosseous pain receptors, but also due to ischemia and mechanical stabilization of the vertebral body. Focal pain at the puncture sites lasting up to 48 hours is commonly observed.
Complication rates associated with vertebroplasty are low and range from 1 to 10%, depending on the initial indications. Potential complications of this procedure can include spinal cord or nerve root compression, rib fracture, pulmonary embolism, epidural abscess, paravertebral hematoma, and sometimes seizures or respiratory arrest due to oversedation.
Percutaneous vertebroplasty has gone a long way from an obscure treatment technique to a highly utilized technique that consistently benefits a significant proportion of patients around the world. The practice of vertebroplasty continually grows both in size and scope, fostering new research, developments, and products.
References
- http://www.hindawi.com/journals/rrp/2011/175079/
- http://www.wjgnet.com/1949-8470/full/v6/i6/329.htm
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3773069/
- http://www.hopkinsmedicine.org/healthlibrary/test_procedures/orthopaedic/vertebroplasty_135,37/
- http://www.biomedj.org/article.asp?issn=2319-4170;year=2013;volume=36;issue=4;spage=162;epage=167;aulast=Lai
- Mathis JM. Percutaneous Vertebroplasty: Procedure Technique. In: Mathis JM, Deramond H, Belkoff SM, ediotrs. Percutaneous Vertebroplasty and Kyphoplasty, Second Edition. Springer Science+Business Media, Inc., 2006; pp. 112-133.
- Jensen ME, Evans AJ. Percutaneous Vertebroplasty. In: Baum S, Pentecost MJ, editors. Abrams' Angiography Interventional Radiology, Second Edition. Lippincott Williams & Wilkins, Philadelphia, 2006; pp. 1110-1130.
Further Reading
Last Updated: May 9, 2021