Introduction
Infection or inflammation
Blockage of the Ducts
Tumors
Vascular Issues
Diseases
Injury to the Organs
Managing Hematospermia
Do Prostatic Conditions Cause Hematospermia?
References
Semen is a fluid that is composed of sperm as well as fluids from the prostate and other glands. The resulting seminal fluid or ejaculate passes through several ducts on its way to the urethra.
First, come the seminal vesicles, accessory sexual organs in the male, located just above the prostate gland and behind the urinary bladder, one on each side. These flat elongated organs produce and store seminal fluid. Their secretion flows into the vasa ampullae.
Sperm is transported from the epididymis of the testis via the vasa deferentia to the vasal ampullae, two tubes passing between the seminal vesicles. The prostate is a gland located at the base of the bladder and wrapped around the bladder neck. The ejaculatory duct is formed within the prostate by the junction of the vasal ampullae and the seminal vesicles. It traverses the prostate to enter the urethra.
The presence of blood in the seminal fluid is often a shocker. It was reported as long back as the time of Hippocrates. About 15% of cases still occur without obvious cause. The rest may be attributed to several causes.
Most patients with blood in the semen are below the age of 40 years, with self-limited episodes of bleeding. Older patients are more likely to have recurrent bleeding episodes.

Image Credit: KateStudio/Shutterstock.com
Infection or inflammation
The most common causes include cysts in the seminal vesicles or ejaculatory duct or bleeding into the duct, making up over two-thirds of hematospermia patients in one study.
Any organs involved in the production and passage of the seminal fluid may become inflamed, including seminal vesicles, vas deferens, testis, epididymis, prostate, or urethra. Irritation of the gland, injury, the presence of calcified foci or stones in the tubular organs, or infections – bacterial, viral, fungal, or parasitic – may cause inflammation. Sexually transmitted diseases (STDs), including gonorrhea, herpes, or chlamydia, can also cause hematospermia.
Blockage of the Ducts
Any obstruction of the ejaculatory duct or cysts formed inside the prostate or seminal vesicles can lead to the appearance of blood in the semen. This is due to the dilatation of the blood vessels near the blocked duct, leading to vessel rupture.
Urethritis is a known cause of hematospermia, more commonly in younger men. Cysts and other benign growths, urethral strictures, or condylomata could account for some cases.
Tumors
The growth of tumors, including benign polyps or cancers of the testis, prostate, epididymis, or seminal vesicles, can cause hematospermia. Still, cancer risk in men who have this symptom remains low, at 3.5%. Cancer is almost never the cause in men younger than 40 years of age and is rare even in older men.
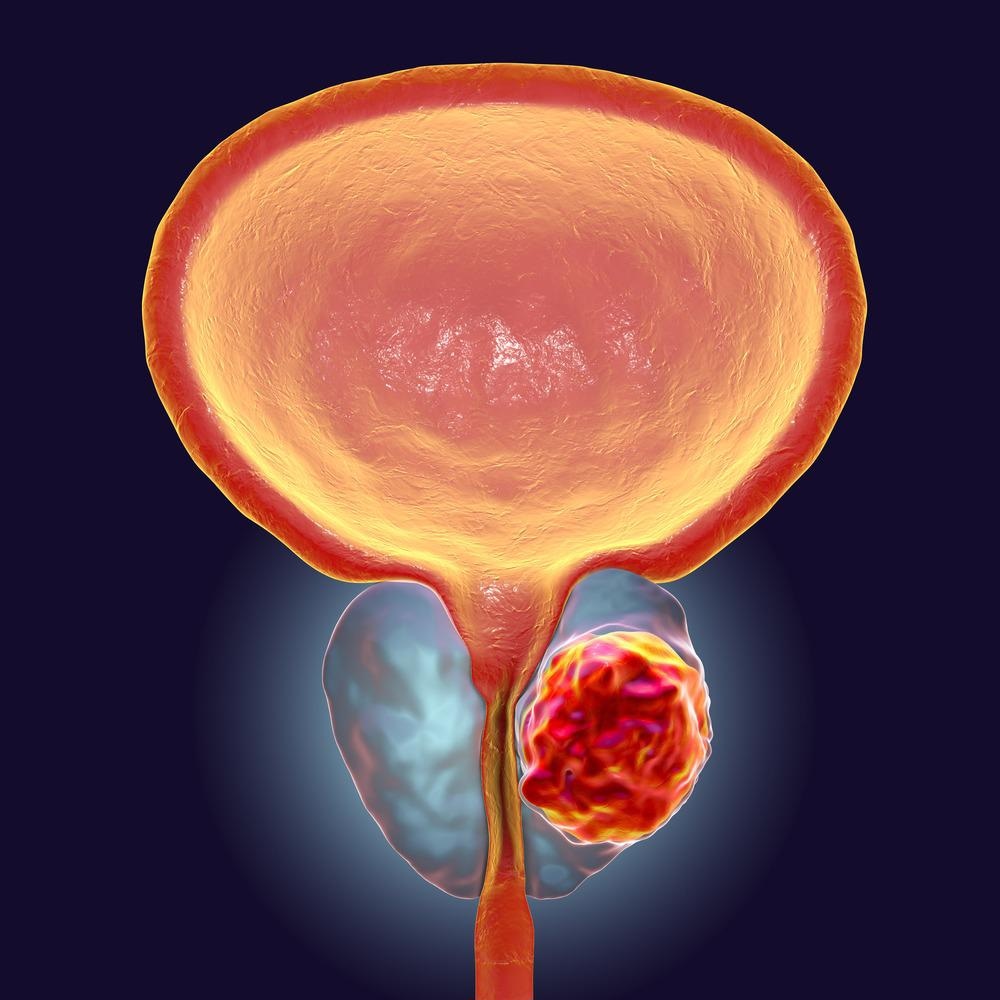
Image Credit: Kateryna Kon/Shutterstock.com
Vascular Issues
Sometimes, the blood vessels supplying or traversing these organs may be abnormally dilated, like telangiectasia or varices, causing blood to leak into the semen.
Diseases
Conditions like hypertension, hemophilia, or chronic liver disease can trigger bleeding into the semen. With hypertension, severe uncontrolled rises in the blood pressure, high serum creatinine, severe proteinuria, and disease of the renal blood vessels are risk factors for hematospermia. Tuberculosis of the vasa deferentia could also trigger hematospermia, as could hyperuricemia.
Injury to the Organs
Hematospermia is primarily due to medical procedures, including prostate biopsy (up to 84% in some studies), radiation therapy, or prostate surgery. Pelvic fracture, injury to the perineal area or the testes, and prolonged abstinence from sexual intercourse are less frequent causes.
Managing Hematospermia
The doctor should investigate the presence of blood in the semen. A careful history, examination of the area, and relevant blood and urine tests will help distinguish the various causes. A check may be ordered to rule out prostate cancer, called the prostate-specific antigen (PSA) test.
In most cases, hematospermia resolves within two months, and if not, further testing may be necessary. Chronic bleeding, or recurrent episodes, should trigger further evaluation.
Ultrasound scanning may be helpful if blood persistently occurs within the prostate. Treatment will depend on the cause, obviously, but a policy of watchful waiting may be adopted if none is found.

Image Credit: Najeeb Designz/Shutterstock.com
Do Prostatic Conditions Cause Hematospermia?
Obstruction of the urethra by an enlarged prostate, as in benign prostatic hyperplasia, can also cause hematospermia.
Prostate biopsy is thought to be most often related to hematospermia, though it is typically self-limited. Prostate cancer is another possible cause but is thought to be still uncommon. Some studies have reported a risk of approximately 14% with this symptom. Still, others have shown it to be present in 6% of men over 40 years who had a raised PSA level or abnormal findings on prostate examination.
Thus, those who have crossed 40 years might find it helpful to screen for prostate cancer if persistent hematospermia presents at any time that is not explained by other causes. These include prostatitis, including bacterial prostatitis; cysts of the seminal vesicles or other accessory glands; stones in the prostate gland; or prostatic cysts.
Red flags indicating the need for further investigation apart from the age include a family history of prostatic cancer, African origin, or features of malignancy like loss of appetite, bone pain, and weight loss.
Those under this age who have one or a very few episodes of hematospermia, and are at low risk for prostate cancer, should be investigated for other common diseases of the genitourinary tract and managed accordingly.
References:
Further Reading
Last Updated: May 31, 2022