The virulence of Ebola is variable and highly dependent on the species or strain of the virus, therefore different species cause somewhat diverse clinical syndromes. When mortality is considered, the highest case-fatality rates (up to 90%) are found with the Zaire ebolavirus species, followed by the Sudan ebolavirus species (40-60%).
.jpg)
Ebola viruses in blood of a patient with Ebola hemorrhagic fever, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
Fatality rates for Bundibugyo ebolavirus species are only 25%, and the single reported person infected with Taï Forest ebolavirus species did not die. Reston ebolavirus species is considered non-pathogenic for man, despite laboratory confirmed infections.
Ebola virus: What is it? We explain in 60 seconds - BBC News
Clinical manifestations
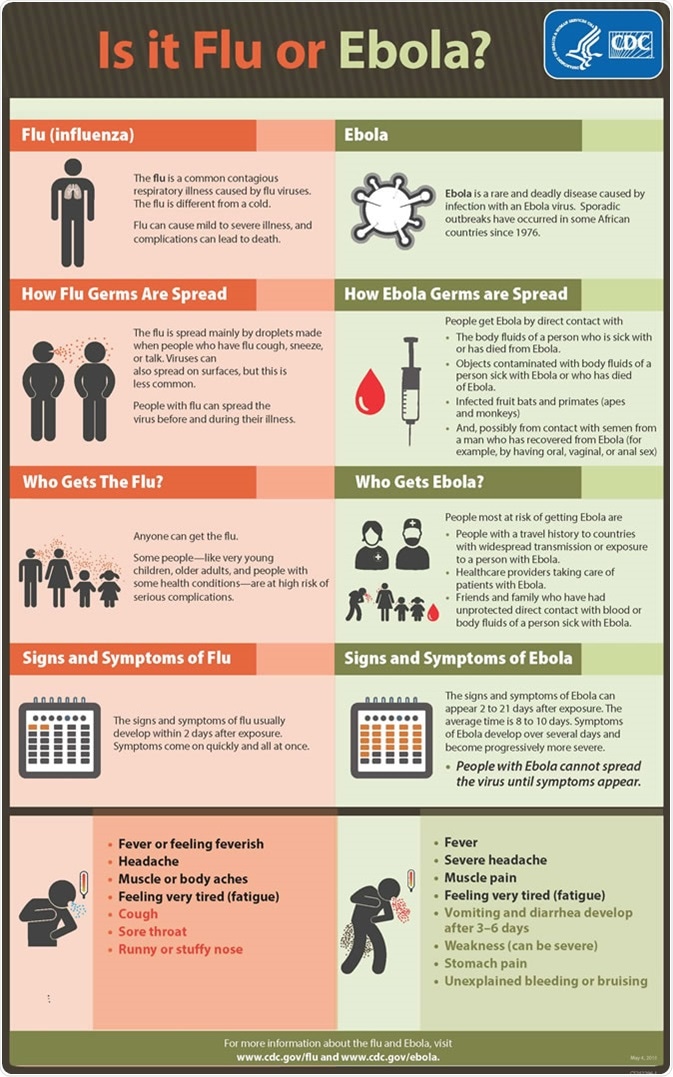
The incubation period for Ebola hemorrhagic fever, which represents the time interval from acquiring the virus to the onset of symptoms, is usually from 2 to 21 days (the average period is 4 to 10 days). The characteristic early symptoms are fever (body temperature greater than 38.6°C or 101.5°F), malaise, chills and muscle pains.
Additional signs and symptoms follow the characteristic involvement of several organ systems in the body. In addition to the extreme fatigue, they include nausea, vomiting, diarrhea and abdominal pain as gastrointestinal manifestations, shortness of breath and chest pain as respiratory manifestations, and headache with confusion and possible coma as neurological manifestations. Between the fifth and the seventh day of the disease papular rash associated with erythema can be observed, which is usually followed by desquamation of the skin in the survivors.
Ebola virus: How is it contracted? BBC News
The development of coagulation abnormalities in Ebola hemorrhagic fever is due to a release of specific tissue factors from monocytes and macrophages infected with the virus. They cause hemorrhagic manifestations during the peak of the disease which include ecchymoses (discoloration from bleeding underneath the skin), petechiae (red or purple spots from bleeding into the skin), uncontrolled oozing of the blood from vein puncture sites, hemorrhages in the mucosa and evidence of visceral hemorrhage after death.
Such hemorrhages can be really severe, but they are present in only half of the infected individuals. That is the reason why some experts prefer to use the term Ebola virus disease instead of the Ebola hemorrhagic fever. Diffuse coagulopathy can occur in later stages of this illness, followed by convulsions, shock and serious metabolic disturbances.
Fatal disease is characterized by the development of clinical signs early in the course of infection, with death typically occurring between day 6 and 16, following the depletion of the circulatory system and multiorgan failure. In non-fatal cases, survivors are usually experiencing fever for several days, when signs of improvement suddenly kick in, typically between day 6 and 11 (in parallel with specific immune response). Recovery is often associated with consequences such as hepatitis, psychosis, or uveitis (inflammation of the middle layer of the eye).
Infection of pregnant women carries an increased risk of miscarriage, and there is a high mortality rate for the children of infected mothers. This could be attributed to the transmission of the virus from the infected mother to the infant during breastfeeding, either by milk or close contact. As pregnant women might suffer hemorrhage due to placenta praevia, abortion or other reasons, it is often difficult to diagnose Ebola in this population.
Laboratory specificities
Low number of white blood cells early in the disease (sometimes even as low as 1000 cells per µL) with concurrent lymphopenia and neutrophilia, low number of platelets (50 000—100 000 cells per µL), the occurrence of atypical lymphocytes, elevated levels of liver enzymes (with aspartate aminotransferase often exceeding alanine aminotransferase), hyperproteinaemia and proteinuria are laboratory characteristics commonly associated with Ebola hemorrhagic fever. However, in the later stages of the disease, secondary bacterial infection can result in a raised number of white blood cells.
Individuals with non-fatal disease mount specific IgM and IgG immunological responses associated with a temporary early and strong inflammatory response. Several inflammatory mediators are triggered, including interferons, interferon-inducible protein 10, interleukins 2, 6, 8 and 10, tumor necrosis factor α (TNFα), monocyte chemoattractant protein 1, as well as reactive oxygen and nitrogen compounds. Such virus-induced expression creates an immunological imbalance that in part contributes to the progression of disease.
Target cells release soluble factors that also contribute to the deterioration of the vascular system, leading to profuse vascular leakage. Prothrombin and partial thromboplastin times are prolonged, while fibrin split products are detectable, indicating diffuse intravascular coagulopathy (DIC) – a life-threatening systemic process resulting in both thrombosis and hemorrhage.
Sources
- www.thelancet.com/.../fulltext
- http://www.who.int/mediacentre/factsheets/fs103/en/
- http://www.cdc.gov/vhf/ebola/symptoms/index.html
- http://www.nejm.org/doi/full/10.1056/NEJMp1405314
- Sanchez A, Geisbert TW, Feldmann H. Filoviridae: Marburg and Ebola viruses. In: Knipe DM, Howley PM, editors. Fields virology. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 1409–1448.
Last Updated: Jun 19, 2019