The pathogenesis of the novel coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its resulting disease of COVID-19 varies greatly, as some individuals with the virus are asymptomatic. In contrast, others suffer from severe manifestations that can include the acute respiratory distress syndrome (ARDS).
Like other kinds of coronaviruses, particularly SARS-CoV and the Middle East Respiratory Syndrome coronavirus (MERS-CoV), the cytokine storm appears to play a direct role in determining the severity of SARS-CoV-2.
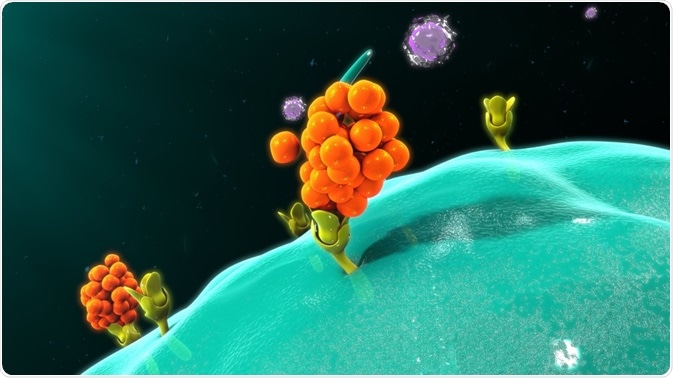 Image Credit: sciencepics/Shutterstock.com
Image Credit: sciencepics/Shutterstock.com
What are cytokines?
Cytokines are small glycoproteins produced by various types of cells throughout the body. Upon their release, cytokines can promote a wide range of functions, some of which involve the control of cell proliferation and differentiation processes, autocrine, paracrine, and/or endocrine activity, as well as regulating immune and inflammatory responses.
Some of the most widely studied cytokines include interferons (IFNs), interleukins, chemokines, colony-stimulating factors (CSFs), and tumor necrosis factor (TNF). The specific actions of each of these important cytokines are detailed in Table 1.
|
Cytokine
|
Actions
|
Types
|
|
Interferons
|
- Regulate innate immunity to viruses and other pathogens
- Antiproliferative effects
|
- Type I (IFN-a and IFN-b)
- Type 2 (IFN-g)
|
|
Interleukins
|
- Regulate immune cell differentiation and activation
- Can have pro- or anti-inflammatory effects
|
|
|
Chemokines
|
- The largest family of cytokines
- Chemoattractants
- Control the migration of immune cells
- Contribute to embryogenesis, the development of the innate and adaptive immune systems and cancer metastasis
|
|
|
Colony-stimulating factors (CSFs)
|
- Associated with inflammation
- Participate in amplification cascade that can promote inflammatory responses
|
- Granulocyte CSF (G-CSF)
- Macrophage CSF (M-CSF)
- Granulocyte-macrophage CSF (GM-CSF)
|
|
Tumor necrosis factor (TNF)
|
- Plays an important role in the cytokine storm
- Excessive production can lead to chronic inflammatory and autoimmune diseases
|
|
Table 1: An overview of the major types of cytokines, as well as their subtypes, and their primary actions throughout the body.
What is a cytokine storm?
The first documented use of the term “cytokine storm,” also referred to as hypercytokinemia, appears in a 1993 article discussing graft-versus-host disease. However, since 2000, cytokine storms have been referenced in various infectious diseases, which is why this term is most commonly used to describe an uncontrollable inflammatory response by the immune system.
In general, acute inflammation begins with five key symptoms including rubor, or redness, tumor, or swelling, calor, or heat, dolor, or pain and functio laesa, which translates from Latin into a loss of function.
Regardless of where the inflammation occurs, increased blood flow will typically follow these symptoms to allow plasma proteins and leukocytes to reach the sites of injury. Although this cellular response is advantageous for host defense against bacterial infections, they often occur at the expense of local organ function.
In addition to this normal response to inflammation, a cytokine storm can also occur. During a cytokine storm, various inflammatory cytokines are produced at a much higher rate than normal. This overproduction of cytokines causes positive feedback on other immune cells to occur, which allows for more immune cells to be recruited to the site of injury, that can lead to organ damage.
One of the most notable clinical conditions associated with cytokine storms includes acute respiratory distress syndrome (ARDS), which has accounted for a significant number of deaths from SARS-CoV-2.
What is ARDS?
The pathogenesis of ARDS begins with inflammatory damage to the alveolar-capillary membrane. Like any other form of acute inflammation, the permeability of the surrounding vasculature, which in this case is that of the lungs, occurs. As the lung permeability rises, protein-rich pulmonary edema fluid is drawn into the lungs, ultimately leading to respiratory insufficiency.
Similar to what was reported during the SARS-CoV and MERS-CoV infections, ARDS is considered to be the hallmark clinical consequence of SARS-CoV-2 by the immune system.
Aside from these viruses, ARDS can also occur as a result of pneumonia, sepsis, pancreatitis, and blood transfusions. ARDS, which is diagnosed when both bilateral lungs infiltrate and severe hypoxemia is detected, is associated with a devastating mortality rate of approximately 40%.

Image Credit: Chinnapong/Shutterstock.com
Cytokine storm in COVID-19
Recent studies on COVID-19 infected patients have shown that these individuals exhibit high levels of both pro-inflammatory cytokines, which include IFN-g, IL-1B, IL-6 and IL-2, and chemokines.
The connection between a cytokine storm and COVID-19 was made when clinicians observed that intensive care unit (ICU) admitted patients had higher levels of CXCL10, CCL 2, and TNF-a as compared to COVID-19 patients that experienced less severe symptoms and did not require admission to the ICU.
Like many other viruses, particularly SARS, MERS, and influenza, the cytokine storm has been used as a warning sign for clinicians to recognize disease escalation. When left untreated, the cytokine storm by COVID-19 produces immunopathogenic damage that not only leads to ARDS in many cases but can also further progress to extensive tissue damage, organ failure, and death.
Treating cytokine storm in COVID-19
Recent research has found that a critical period of 5-7 days exists between the time of COVID-19 diagnosis and multiple organ dysfunction syndrome (MODS). Whereas about 80% of patients tend to improve after this window, about 20% of patients will experience severe pneumonia and approximately 2% will ultimately succumb to this virus.
A huge range of anti-inflammatory therapies are being looked at for treating the cytokine storm in COVID-19. To directly reduce the deleterious effects that the cytokine storm can have on individuals who test positive for COVID-19, researchers have recommended that immunotherapy is administered at the time of cytokine storm diagnosis.
Some notable immunotherapeutic strategies that have been proposed for this purpose include neutralizing antibodies, which can be obtained from the plasma of patients who previously survived COVID-19 infection, IFN inhibitors, and oxidized phospholipid (OxPL) inhibitors, and sphingosine-1-phosphate receptors 1 (S1P1) antagonists.
Further clinical studies must still be performed to fully evaluate the ability of these treatment options to successfully inhibit the cytokine storm induced by COVID-19.
References
- Coperchini, F., Chiovato, L., Croce, L., Magri, F., & Rotondi, M. (2020). The cytokine storm in COVID-19: An overview of the involvement of the chemokine/chemokine receptor system. Cytokine & Growth Factor Reviews 53; 25-32. doi:10.1016/j.cytogrf.2020.05.003.
- Cron, R.Q. (2021). COVID-19 cytokine storm: targeting the appropriate cytokine. The Lancet Rheumatology. doi:10.1016/S2665-9913(21)00011-4
- Song, P., Li, W., Xie, J., Hou, Y., & You, C. (2020). Cytokine Storm Induced by SARS-CoV-2. Clinica Chimica Act. doi:10.1016/j.cca.2020.06.017.
- Sun, X., Wang, T., Cai, D., Hu, Z., et al. (2020). Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine & Growth Factor Reviews 53; 38-42. doi:10.1016/j.cytogfr.2020.04.002.
- Tisoncik, J. R., Korth, M. J., Simmons, C. P., Farrar, J., et al. (2012). Into the Eye of the Cytokine Storm. Microbiology and Molecular Biology Reviews. doi:10.1128/MMBR.05015-11.
Further Reading
Last Updated: Jun 23, 2022