Head trauma refers to any damage to the scalp, skull or brain caused by injury. Head injury may be classified in various different ways according to the type of injury, which structures in the head are damaged or how severe the trauma is.
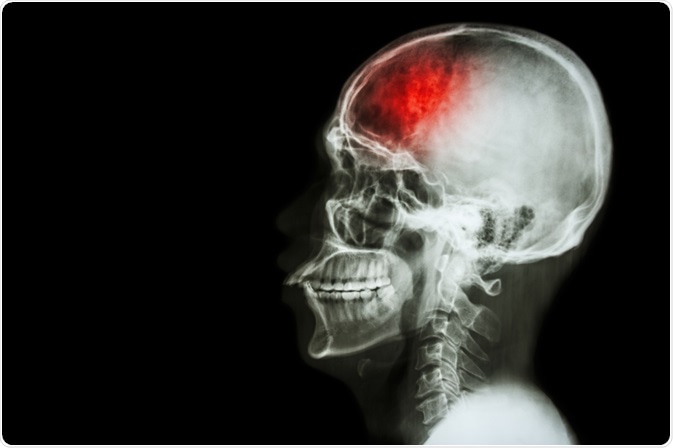 Image Credit: Puwadol Jaturawutthichai / Shutterstock.com
Image Credit: Puwadol Jaturawutthichai / Shutterstock.com
Closed or open injury
One way head injuries are classified is according to whether the injury is open or closed.
Closed injury
A closed injury refers to damage that does not break the skull or penetrate the brain tissue. Although the skull is not broken, this type of injury can still cause brain damage in the form of swelling or bruising, for example.
Open injury
An open injury refers to damage that penetrates the skull causing problems such as bleeding in the brain, skull fracture or the pressing of bones against structures in the brain. This type of injury is more likely to occur when a person is moving at high speed, when colliding with a windscreen during a car accident, for example. A gunshot to the head would be another example.
Concussion
This form of head injury occurs when the brain is shaken, which may or may not involve a blow to the head. The effects of concussion range from headache to loss of consciousness.
Primary or secondary lesion
Head injury may be classified according to the type of lesion involved. The two main types of lesions that occur in head trauma are primary lesions and secondary lesions. Primary lesions occur as a direct result of initial injury to the head causing displacement of the physical brain structures. Secondary injuries occur over time and may involve several cellular processes rather than mechanical damage. Secondary lesions can occur as a result of the primary lesion or they may be unrelated to it.
Primary injury
Primary injury is an injury that occurs as a direct result of the initial head trauma. Examples of primary injury include contusion (bruising or hematoma), vascular damage, and axonal shearing (torn and stretched nerve axons). Primary injury can damage the blood–brain barrier and meninges and lead to neuronal death, which may occur in a random manner. Different brain areas may sustain different levels of damage depending on their sensitivity to mechanical loading. Two main causes of primary injury are a blow to the head received by an object and the brain hitting against the inside of the skull.
Secondary injury
A secondary injury is one that is not mechanically induced but occurs as a result of the primary injury causing complications such as inadequate blood flow in the brain (ischemia), reduced availability of oxygen (hypoxia) in the brain, low blood pressure, increased intracranial pressure (pressure inside the skull), or swelling in the brain (cerebral edema). Other causes of secondary injury include meningitis, brain abscess, increased carbon dioxide levels, free radical damage, and acidosis.
Head trauma severity
Head trauma is also classified according to how mild or severe it is, which affects how the injury is managed.
Mild injury
Mild head injuries are common amongst all age groups. Symptoms are usually short-lived, with no permanent damage caused. Examples of symptoms include:
- Mild headache
- Poor balance or trouble standing
- Confusion
- Nausea
- Dizziness
- Small cut or bump
- Ringing in the ear
- Mild blurring of the vision
- Temporary amnesia
People who experience any of these symptoms after a mild knock or blow do not usually require treatment, but should visit their local accident and emergency department for a check-up.
Overview of Traumatic Brain Injury (TBI)
Severe head injury
Some of the indications of severe head injury include:
- Bleeding from deep wounds in the scalp
- Unusual eye movement
- Loss of consciousness
- Inability to focus
- Poor muscle control
- Vomiting
- Convulsion
Serious head injuries require immediate medical attention so that any bleeding or brain damage can be accurately assessed and treated.
Treatment depends on what type of injury a person has and their overall state of health and ability to withstand treatment. Treatments range from drug therapies to address seizures or bleeding, through to surgery to reduce bleeding, swelling in the brain or pressure inside the skull.
References
Further Reading
Last Updated: Dec 21, 2022