Status epilepticus (SE) is an extremely serious and often fatal medical emergency. It may be defined as a continuous seizure which lasts for 30 minutes or more, or as 2 or more seizure episodes without the patient recovering full consciousness in between any 2 episodes.
It is thought to be due to the lack of efficacy of GABA-ergic activity which is typically responsible for terminating abnormal electrical activity in the brain. Once SE is in progress, it should be treated by benzodiazepines, with fosphenytoin being added if required. If the patient does not respond, but has persistent seizures, a second-line drug is administered, such as a barbiturate, Propofol, sodium valproate, levetiracetam or topiramate, according to the situation and the facilities available. The patient must also be monitored for hemodynamic collapse.
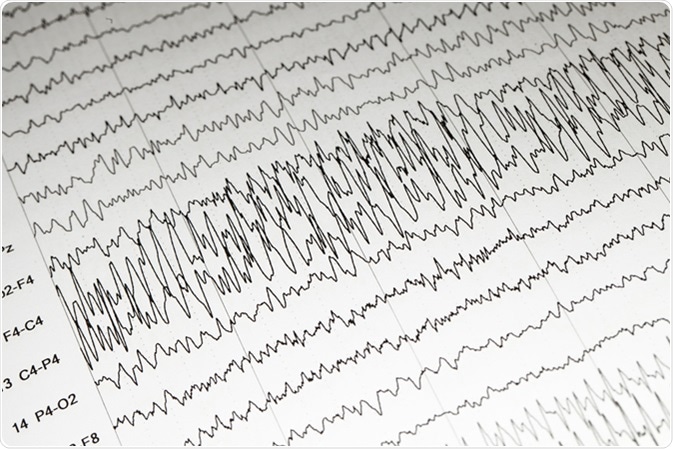
EEG wave background, Status epilepticus wave form. Image Credit: Chaikom / Shutterstock
Diagnosis
SE was first discussed at length at a meeting in Marseilles in 1962, and it was pointed out that it exists in many different forms. It also defined SE as any seizure that persists long enough or is repeated often enough to constitute a fixed state of seizures. This definition persisted with little modification until 1993, and at this time the American Epilepsy Society Working Group on Status Epilepticus added a temporal qualification, namely, seizure duration of 30 minutes or more, to the above. The reason for selecting such a time period was based on the concept that prolonged seizure activity could potentially cause brain damage.
Currently, a duration of not more than 5 minutes has been proposed, based on the finding that most seizures last less than a couple of minutes, and those which are prolonged beyond this duration rarely terminate spontaneously. Secondly, these prolonged seizures are also refractory to anti-epileptic drugs and are more likely to cause neuronal damage. Moreover, it is not feasible in any clinical situation to wait for 30 minutes before treating the condition as SE, and the seizures become unresponsive to treatment during this time. For this reason, it is deemed wise to wait not longer than 2 minutes before treating a convulsive episode as SE.
Recognizing and Treating Status Epilepticus
Classification of SE
SE has as many types as the broad seizure classification contains. It may be first categorized as convulsive and non-convulsive SE.
Convulsive SE (CSE)is further subdivided into:
- Tonic-clonic SE
- Tonic SE
- Clonic SE
- Myoclonic SE
Generalized tonic-clonic SE is the type most commonly found to occur in clinical practice. It is accompanied by hyperactivation of the autonomic nervous system with hypertension, hyperglycemia, salivation and sweating, with steep increases in temperature way beyond normal range (hyperpyrexia). Cerebral blood flow is increased during this phase.
Non-convulsive SE (NCSE) is a state in which the brain shows almost constant and generalized electrical activity consistent with seizures for 30 minutes or more, but without seizures being manifested.
The patient shows disorientation or other abnormal mental states or may not respond to any stimuli. Other signs include aberrations of eye movement, and some type of response to anticonvulsant therapy. This may be the result of treating CSE or the only manifestation per se.
For this reason, if a person continues to display unusually long periods of confusion or goes into a coma following a seizure, an electroencephalogram (EEG) is appropriate to confirm this diagnosis. NCSE may be subdivided into absence SE and complex partial SE.
It is thought that NCSE often reflects the failure of autoregulation of cerebral blood flow with a fall in cerebral circulation and increased intracranial tension, with a reduction in systemic blood pressure. The presence of electrical seizure activity unaccompanied by major seizure movements is thought to be due to electromechanical dissociation.
A third state called epilepsia partialis continua is diagnosed when the patient suffers from repeated partial seizures such as focal motor, sensory or functionally impaired symptoms but retains full awareness.
EEG-Based Classification
Five patterns are seen on EEG:
- Separate episodes of seizures
- Merging of seizure activity
- Continuous seizure activity
- Continuous seizures with flat periods intervening
- Seizure-like discharges occurring regularly against a flat background
Variants of SE
SE that persists despite standard treatment is seen in up to about 9-30% of patients and has a worse prognosis. This is called refractory SE and is defined when SE persists for more than 60 minutes after administering a benzodiazepine plus another antiepileptic drug in standardized loading dosages.
Malignant SE, on the other hand is defined when aggressive treatment with anticonvulsants and even anesthetic agents fails to arrest the seizure and is more common between 18 and 50 years and especially in the presence of encephalitis.
Treatment
Adults with CSE are treated with parenteral benzodiazepines or phenobarbital at first, monitoring the respiratory and pulse rate. Children receive a benzodiazepine. Phenytoin or preferably fosphenytoin is an alternative.
Further Reading
Last Updated: Feb 27, 2019