The balloon occlusion test (BOT) is a medical technique that is employed to determine if an artery can be transiently blocked without significantly affecting blood flow to the organ concerned. It is conducted before sacrificing the artery, and helps to predict the outcome of some types of vascular surgery, as well as to decide the best course of treatment.
The BOT is routinely done and widely accepted in the management of patients affected by aneurysms and those with tumors of the head and neck, as well as intracranial tumors. It is especially employed in the latter cases for those patients who have a high chance of requiring prolonged intraoperative internal carotid artery (ICA) occlusion.
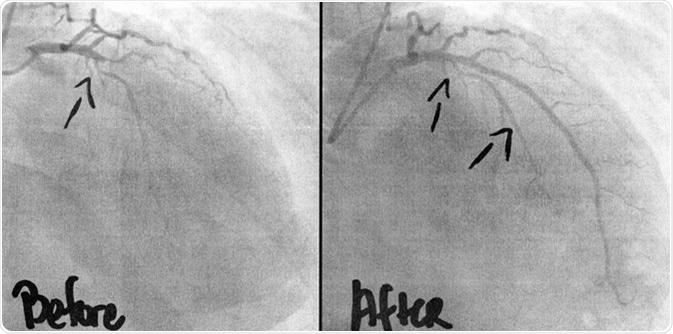
Coronary Angiogram imaging, before, and after 3 stents, and ballooning of two occlusions was performed intravenously by a cardiac surgeon. A life saving intervention for the 54 year old man. Image Credit: KellyNelson/ Shutterstock
The Importance of the BOT
It is imperative to conduct a BOT before such surgeries, because surgeons must be able to ascertain that there is sufficient collateral circulation to the brain, for example, before commencing deconstructive procedures to treat vascular diseases. Insufficient collateral circulation may lead to an iatrogenic stroke during endovascular procedures that deconstruct the vessels. X-rays are necessary in addition to the use of specialized dyes that are used to generate detailed images of the vascular network. In addition to X-rays and dyes, a small inflatable balloon is needed to block the flow of blood within the vessel being studied.
The History of Carotid Occlusion
There is a significant risk of intraoperative bleeding when managing tumors of the head and neck, as well as intracranial vascular diseases. In order to reduce this risk during surgical procedures, carotid occlusion may be necessary. Historically, several methods have been applied to accomplish this feat. These include occlusion done under local anesthesia with removal bands, and the application of manual percutaneous pressure.
If the patient did not exhibit any signs or symptoms during these tests, then they were considered negative. However, there have always been some cases in which neurological deficits of late onset occurred.
Thanks to advancements in medicine, science and technology, that allowed for the measurement of cerebral flow during occlusion, it is possible to immediately detect subtle inadequacies in collateral circulation, which could otherwise present as neurological damage of late onset. Single-photon emission computed tomography (SPECT) imaging with the help of Tc-ECD or HMPAO is an example of a widely used method that may be employed with the BOT. This can generate information to guide surgeons in their approach to treating their patients, and help them to determine how far they may proceed with their operations.
Summary of the BOT Procedure
An angiogram is required before a BOT can be carried out. Angiograms are examinations of blood vessels performed with the use of X-rays and a special dye to visualize the vessels. Once the pictures are obtained, a catheter with a built-in balloon is advanced through to the blood vessel of interest. After it is in position, it is inflated to block the flow of blood.
Aortic Balloon Occlusion REBOA
Before this disruption in the flow of blood, patients are given medication to prevent clotting of blood once the flow is interrupted in the vessel of interest.
During the inflation of the balloon, a series of clinical tests, involving neurological function, among others, is conducted. In the presence of good collateral circulation, no neurological deficits are noted during this time, and the BOT is considered to be negative, which indicates arterial sacrifice for surgical management is possible. However, if the patient develops any signs and/ or symptoms of transient neurological dysfunction during the BOT, the balloon is immediately deflated, upon which the indicators of poor collateral circulation usually resolve straightaway.
Further Reading
Last Updated: Nov 27, 2018