A sclerotomy is a surgical procedure that creates an incision in the sclera of the eye. This procedure is normally performed to correct scleral defects that arise as the result of ocular diseases such as glaucoma.
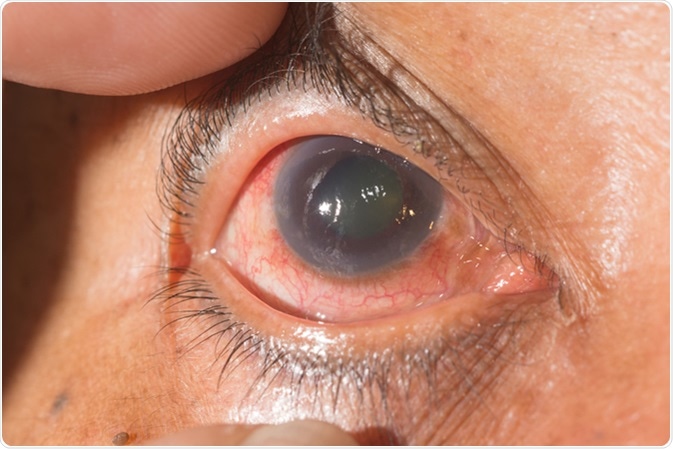
Close up of the neo vascular glaucoma during eye examination. Image Credit: ARZTSAMUI / Shutterstock
Performing a Sclerotomy
Transconjunctival sutureless vitrectomy
Sclerotomy can be done in several different ways depending on the disease being treated. One method is referred to as a transconjunctival sutureless vitrectomy (TSV), which involves removing some of the vitreous humor of the eye without using sutures to close the incision up. After this procedure, the eye is massaged to aid the healing process. While performing the surgery, intraocular manipulation such as moving the vitreous cutter within the vitreous cavity is a factor in increased deformation of the sclerotomy. More time is required to treat such a deformation.
High-frequency deep sclerotomy
Another method of sclerotomy is high-frequency deep sclerotomy (HFDS). It is a minimally invasive procedure that has good results. Unfortunately, the nature of the procedure limits manipulation of the scleral and conjunctival tissues. HFDS uses a diathermic high-frequency dissection 19-gauge probe to introduce a 500 kHz current through a 0.3 mm x 0.1 mm tip. Six pockets are made in the sclera using the probe, which allows two incisions to be made. The probe is inserted into one of the incisions allowing for the zone of interest to be visually inspected. The probe is now pushed in one more millimetre into the sclera to make a deep sclerotomy.
Full-thickness sclerotomy
Uveal effusion syndrome (UES) is a disorder that is characterized by the build-up of fluid that has escaped from the choriocapillaries into the nearby free space. This results from compressed vortex veins caused by a thickened sclera. The outcome is very serious ocular abnormality. One method of treatment for UES is decompression of the vortex veins via scleral resection (eyeball shortening) with sclerostomy (a small opening in the outer covering of the eyeball). This treatment also reduces the intraocular pressure (IOP) in patients undergoing ocular surgeries.
Full-thickness sclerotomy can also be used to treat other disorders of the eye. Previous studies have shown the significant effectiveness of full-thickness sclerotomy for disorders such as retinal detachment, thickening of the sclera, subretinal fluid movement, and sclerosis of the lens. These studies showed varied results that show the effectiveness of full-thickness therapy can range from mildly effective to extremely effective depending on the disorder for which it was used.
DEEP SCLEROTOMY (3413)
Complications
Complications can arise following a sclerotomy, such as leakages and post-operational hypotony (low IOP). These are risk factors for the development of acute-onset endophthalmitis (inflammation of the interior of the eye) which can lead to loss of vision. Using oblique sclerotomy incisions instead of conventional incisions reduces the incidence of leakage due to their self-healing effects.
Vitreous incarceration traps the vitreous within the incision site. This can complicate surgeries and lead to further damage of the eye following a sclerotomy. The complications that are caused by this include fibrous ingrowth within the eye, macular edema, and retinal tears.
Conclusion
Due to the differences in the way different eye diseases manifest, many varied sclerotomy procedures exist. The procedure that is used depends on many factors, including the age of the patient, the disease, and its severity of the disease. Once a sclerotomy procedure has been performed, several complications may arise which can further damage the eye, making the surgery ineffective. Fortunately, there are methods that can be used to reduce the risk of further damage due to sclerotomies. Researchers and healthcare professionals have innovated many methods to increase the efficiency of sclerotomy procedures, which will only increase in the future.
Further Reading
Last Updated: Oct 15, 2018