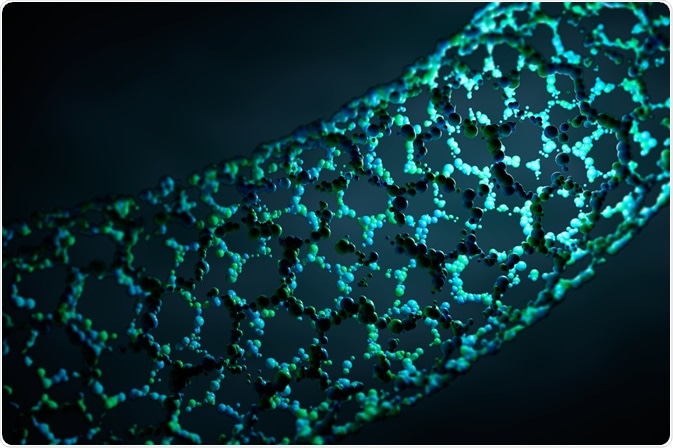
Carbon nanotubes (CNTs) are hollow structures made up entirely from carbon. The walls of the carbon nanotube are just one atom thick, created by rolling sheets of graphene into a long tube with aspect ratios as large as several million to one. Due to their size, CNTs have been investigated for their ability to deliver immunotherapies.
 FoxStudio | Shutterstock
FoxStudio | Shutterstock
Why carbon nanotubes?
The high aspect ratio shape of CNTs allows for relatively easy entry into cells while possessing a large surface area to volume ratio and highly functional carbon surface chemistry. This allows both the outer and inner surface of the CNT to be modified with targeting ligands and chemotherapeutic drugs, among other payloads such as immunotherapeutic proteins.
The unique physical properties of CNTs, most notably high thermal and electrical conductivity, also make them excellent candidates as photothermal therapy agents. They are highly stable and, thus, are able to exist in the blood plasma for protracted periods of time, ensuring that drug payloads survive in the body for long enough to reach their target destination. The delivery of large quantities of a drug to the target by such a vehicle also ensures that the drug or other efficacious molecule is present in sufficient quantity to exert a significant effect.
How does immunotherapy work?
When cells become cancerous, they tend to possess genetic mutations that result in uncontrolled growth, coupled with changes that render them unnoticed by the immune system. Cells bearing dangerous mutations generally also present foreign antigens on the surface of the cel, and subsequently generate proteins in unusual proportions.
These changes should be recognized by white blood cells as aberrant, leading to the destruction of the cell. However, multiple resistance strategies are frequently developed in cancer cells that lead to immune evasion, the creation of tolerance, or the disruption and prevention of white blood cells from fulfilling their function.
Immunotherapy aims to counter these resistances through the augmentation of the body’s natural defenses; one salient example of immunotherapy is vaccination. In this approach, antigens specific to the cancer being vaccinated against are given to the patient in order to stimulate the production of T cells that will attack the cancer cells. This method is currently not particularly effective, as strategies of resistance to T cells expressed by tumors must still be overcome.
Oncolytic virus therapy utilizes engineered viruses that are intended to replicate within and destroy cancer cells only. They may be made to express particular cytokines that encourage the activity of T cells towards the cancer cell, or improve the recruitment rate of such biomolecules.
T cells that have been directly modified to recognize the antigens expressed by cancer cells are also in development, and promise to provide a direct ‘boost’ to the immune system of an individual with malignancies that have developed resistances to their own immune system.
Immune checkpoints regulate the immune system and prevent white blood cells from over-acting and destroying healthy cells. Conversely, malfunctions in the operation of immune checkpoints may lead to cancer cells being ignored by the immune system. Immune checkpoint blockade drugs side-step this dysfunction and encourage the activity of T cells.
Which immunotherapy agents can CNTs deliver?
CNTs are able to carry drugs and biomolecules in a variety of ways, including covalent and non-covalent bonding methods and entrapment within the hollow center of the tube. Many types of proteins in particular have been bound to CNTs for immunotherapy purposes, especially antibodies.
For example, the surface of CNTs have been coated with antigens also expressed by the cancer cells, acting as an ‘artificial antigen presenting cell’, which triggers an immune response and, therefore, the production of T cells that specifically target that antigen.
Further Reading
Last Updated: Mar 26, 2019