Antigenic drift is the accidental alteration of genes encoding antigens. It typically occurs in viruses and enables the pathogen to evade the immune system, triggering an infection once more.
Credit: Kateryna Kon/Shutterstock.com
Antigens are molecules which can be bound by immune cell receptors in order to trigger an immune response. This mechanism of binding and recognition is used to detect threats to the body, including bacterium, viruses and various chemicals. The cells of the body also display antigens, which enable them to be distinguished from foreign material.
What is antigenic drift?
Receptors of the immune system bind to foreign antigens specifically, like a key inserting into a lock, which triggers an immune response to eliminate the threat. Once the infection is resolved, the body can produce many more of these specific receptors which can detect these specific antigens upon reinfection.
This functions as an acquired immune response, preventing future infections of the same antigen. If the same antigen is detected, the body can make the specific receptor very quickly, producing a fast and effective immune response, and preventing a second infection.
Vaccinations work with this acquired immune response, stimulating the production of receptors without the individual having to face the primary infection. Non-threatening antigens are introduced into the body which stimulates the production of specific immune receptors. Therefore, if the actual antigen is detected, an acquired immune response can be mounted and the body can fight off the infection more effectively.
However, both vaccinations and the acquired immune response can only function if the antigenic structure remains the same. If the structure is altered, such as in antigenic drift and antigenic shift, then the highly specific receptors will no longer bind and so the acquired immune system will no longer be able to detect the threat.
An individual who has previously suffered with a specific viral infection, for example, can become ill for a second time. Therefore, altering the structure of surface antigens provides a potential mechanism for the evasion of the immune system by pathogens.
Antigenic drift and influenza
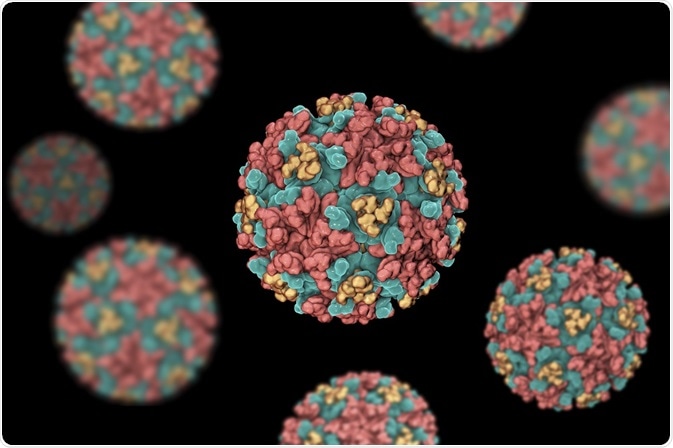
The surface antigens of influenza include hemagglutinin (HA) and neuraminidase (NA). Hemagglutinin binds to epithelial cells and allows entry of the virion, whereas NA functions in the process of new virions budding from body cells.
When influenza replicates its RNA to reproduce, errors can be made which lead to a mutation. Around 1 in 10000 nucleotides are transcribed incorrectly, which roughly is the length of the influenza genome, meaning that there is approximately 1 mutation every time influenza replicates. RNA, unlike DNA, lacks the ability to fix these mutations as it does not have proofreading enzymes, and therefore these errors lead to a small but permanent change in the genetic code.
This means that every time influenza replicates, the progeny are slightly different and can have slightly different HA and NA. Over time these differences accumulate and produce antigens which are substantially different to their ancestors. Therefore, their antigens “drift” which means they can no longer be detected by the acquired immune system of the body.
An individual who has previously suffered from one strain can then be reinfected as the body has no way of detecting that this is the same infection.
Antigenic drift is a major problem in the design of vaccinations, particularly in influenza A. The slight changes in antigen structure mean that previous vaccines are no longer viable and new vaccines are constantly required. In the future, vaccines which can bind to different variants of HA and NA may provide protection against antigenic drift.
Influenza: Get the (Antigenic) Drift
Further Reading
Last Updated: Feb 26, 2019