Diabetic mastopathy (DMP) is usually discovered by the patients themselves and they describe it as an irregular and painless lump. After informing their family physician, screening procedures for breast cancer will begin, which includes mammograms and breast ultrasound studies.
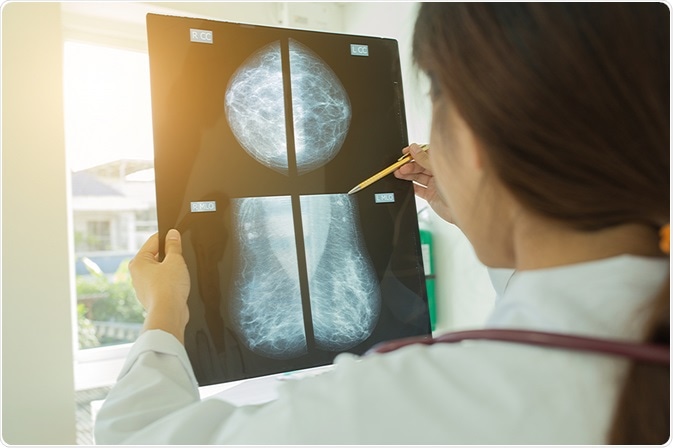 Image Credit: Chompoo Suriyo / Shutterstock.com
Image Credit: Chompoo Suriyo / Shutterstock.com
Once imaging studies are over and if the findings are inconclusive, a biopsy is performed to confirm the findings and rule out breast cancer. Histological analysis is an important method that helps differentiate DMP from breast carcinoma.
DMP lesions are of various sizes and can be present in any of the quadrants of the breast, though it is more common for them to appear in the subareolar region. Specific features of DMP are generally not clear from imaging studies, though a discrete mass with pronounced acoustic shadowing is evident in ultrasonograms. Also, mammograms can reveal homogenous and dense glandular tissue with no signs of microcalcification or architectural distortion. Unfortunately, radiologic and clinical studies do not help much in differentiating DMP from breast cancer.
The radiographic features of DMP that may be used in the diagnosis of diabetic mastopathy are outlined below.
Mammography in diabetic mastopathy
Mammographic findings of breast masses usually show poorly defined lesions often surrounded by glandular tissue. This makes mammographic studies more difficult in the case of DMP.
Breast ultrasound in diabetic mastopathy
An ultrasound of the breast often reveals shapeless masses that are hypoechoic with clear posterior acoustic shadowing. Sonographic features often mimic features of more severe cases such as breast carcinoma.
Breast MRI in diabetic mastopathy
MRI of the breast leads to a range of findings from less diffuse contrast material enhancement to rapid, intense enhancement that is indistinguishable from breast carcinoma.
Clinical findings are mostly inconclusive after imaging and these masses are more often misdiagnosed by physicians as breast carcinoma. Identifying this condition precisely and differentiating it from carcinoma is critical in avoiding unnecessary surgical procedures.
DIABETIC MASTOPATHY BY DR WAFAEY BADAWY
Histological examination in diabetic mastopathy
Histological study is the only way to confirm the diagnosis of DMP. Histological examination of DMP masses shows firm, white, homogenous lesions that are separated to an extent from the surrounding breast tissue. There is clear fibrosis and the presence of lymphocytes around the ducts and lobules. Very little to no adipose tissue or cellular materials are seen during histological analysis. Cytological images in the case of DMP show extensive infiltration of the ducts, vessels, and lobes by mature lymphocytes. General pathognomonic findings specific to DMP include epithelioid fibroblasts, keloidal fibrosis, and lymphocytic ductitis or lobulitis.
Sampling using fine needle aspiration is difficult because DMP masses are usually resistant to needle passes. Also, the cellular yield is usually insufficient for diagnostic needs in up to 70% of patients with DMP. Hence, core biopsy is a better approach in terms of diagnostic yield.
Differential diagnosis in diabetic mastopathy
Pathologists need to be very careful during the diagnosis of DMP as it is easy to misdiagnose and it can recur after some time. As DMP masses look similar to those in breast carcinoma, pathologists and radiologists should be able to differentiate between the two. A correct diagnosis can save patients from unwanted surgical biopsies. No evidence exists to suggest that DMP leads to breast cancer or stromal neoplastic diseases.
Careful correlation of the medical history of the patient with the radiological, physical, and pathological investigations is very important for the diagnosis of DMP. Post confirmation of diagnosis, the patients can be monitored by fine-needle aspiration cytology (FNAC), which is a diagnostic method for investigating masses or lumps.
References
Further Reading
Last Updated: Jan 28, 2021