The need to avoid immunosuppression is often the driving force behind research into alternative therapeutic options for the treatment of a range of diseases.
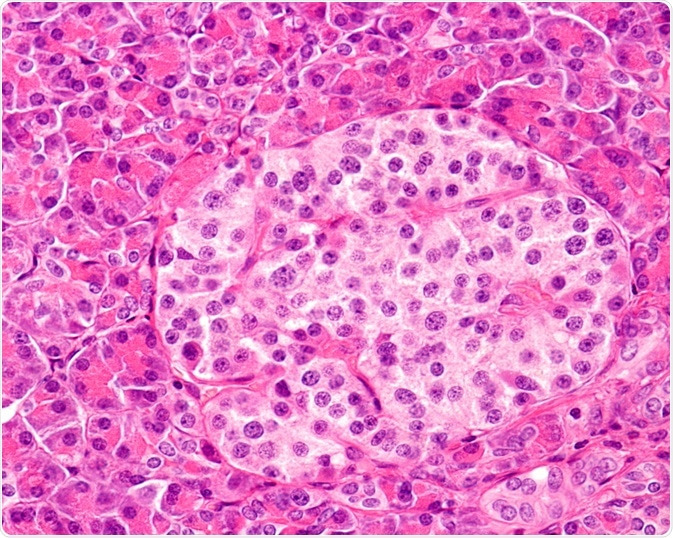
Image Credit: Jose Luis Calvo/Shutterstock.com
One such disease is type I diabetes, which develops as a result of immune cell-mediated destruction of the pancreatic B cells.
Encapsulation and tolerance induction are two means of circumventing the need for immunosuppression.
Stability, Resistance, and Integrity: The Benefits of Encapsulation
In encapsulated islet therapy, beta cells in patients with T1DM are replaced with immunoprotective islets derived from healthy donors. These donor islets are delivered inside selectively permeable alginate hydrogel microcapsules.
This approach has been shown to restore normal glycaemic levels or reduce insulin dependency in diabetic rodent models and primates in the absence of immunosuppressive drug administration. However, clinical trials of such encapsulated islet cells have not yielded good results to date, so application to humans has been limited.
To address these concerns, a team lead by Professor Arifin from the Johns Hopkins University have devised a means of ‘hot-spot’ imaging of encapsulated islet cell transplants in vivo using 19F MRI.
A decrease in 19F MRI signal indicates capsule rupture whereas a strong intact fluorocapsule projected a stable 90-day long signal in vivo. As such, these fluorocapsules present a clinically relevant means of monitoring and predicting islet graft rejection and future failure of encapsulation-based therapy.
The success of encapsulated islet therapy is hinged on their mechanical stability; ruptured capsules result in exposure to the hostile environment of the pancreas.
Capsules must be able to withstand the shearing force and changing size of the microenvironment of the graft. Methods to evaluate this property are currently not clinically relevant nor non-invasive, with current methods restricted to in vitro rotational stress, compression and, osmotic pressure testing.
Improving Encapsulation Research Using Fluorophores
To improve the efficacy of encapsulation research, a team from John Hopkins University has developed a clinically relevant means of testing the integrity of encapsulated islet cells using fluorocapsules.
To prepare the capsules, the team added perfluoro-15-crown-5-ether (PFC) to the alginate hydrogel for fluorocapsule production. PFC produces a single MRI peak that generates background noise-free ‘hot-spots’ on 19F MRI.
The team compared two types of fluorocapsules: strong, dual-layer cross-linked and alginate gelation and weak single layer fluorocapsules subject to alginate lyase-induced rupture. The team also performed bioluminescent imaging (BLI) to determine how the magnitude of the 19F MRI signal reflected islet cell viability.
After transplantation into mice, the 19F MRI signal of capsules was shown to remain stable for up to 90 days, which corresponded to the total intact fluorocapsules. Rupturing of capsules by an alginate lyase resulted in the dissipation of the 19F MRI signal 4 days later.
Additional testing of a fluoroencapsulated luciferase-expressing mouse insulinoma cells that were implanted into autoimmune mice revealed that the 19F MRI signal decreased sharply following capsule rupture induced by alginate lyase.
This dissipation is caused by the exhalation from the body. This coincided with bioluminescence image decline and corresponded to a measure of cell viability in vivo. The dissipation of the 19F MR signal is therefore used as an imaging biomarker for the loss of immuno-protection from compromised encapsulated cell therapy.
This proof-of-concept study provides a means of testing the stability of encapsulated islet cell transplants in vivo using 19F MRI. Ruptured islet cells can be monitored by viewing the 19F MRI signal, which is seen to dissipate.
The researchers concluded that “The use of fluorocapsules may provide a clinically relevant, quantitative and non-invasive strategy to monitor the mechanical stability of the capsules in vivo in a serial and real-time fashion.” As such, capsule integrity is shown to be essential for preserving transplanted cell survival, and thus efficacy of transplantation as a means of immunosuppressive-free therapy.
Further Reading
Last Updated: Mar 12, 2020