Skip to:
Thalidomide was first marketed to health professionals as a sedative. However, its use rapidly increased amongst pregnant women due to the drug’s ability to alleviate morning sickness.
Soon after its rise in popularity, medical professionals began to note a series of congenital mutations in children born from mothers who used the drug during pregnancy, resulting in the thalidomide tragedy known today.
In more contemporary times, thalidomide has become renowned for its effectiveness in treating malignant and inflammatory diseases.
What is Thalidomide?
Thalidomide was first developed by CIBA, a Swiss pharmaceutical company in the early 1950s, and subsequently introduced as Contergan by Chemi Grunenthal.
The drug was initially advertised as a sedative which would allow users to undergo a deep sleep in the absence of a hangover and with a reduced risk of developing drug dependency. At the time, basic testing was done on the drug, and it was considered not to have any toxic effects on humans.
However, unlike today’s level of rigorous testing, the drug was not analyzed for any potentially dangerous teratogenic effects.
Following its release, the drug became popular as a morning sickness remedy for pregnant women due to its anti-emetic effects. This increase in use for pregnant women was aided by the fact that the drug could be obtained without a prescription, and was affordable.
However, following its widespread use in Japan, Australia, and Europe, practitioners began to notice links between mothers who had taken thalidomide and the presence of congenital mutations in their children.
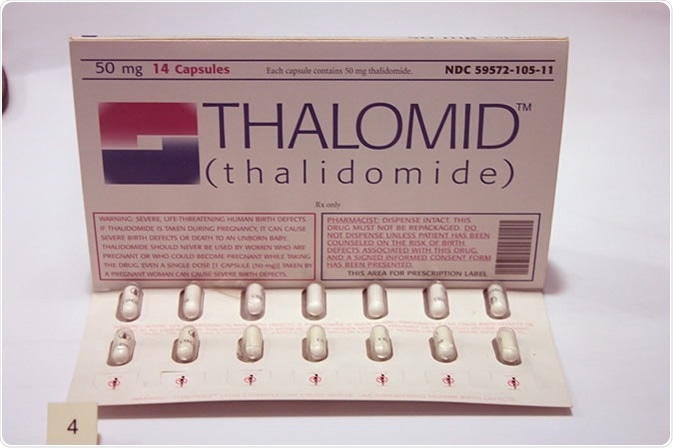
Pack of Thalidomide tablets circa 2006 or later. Image Credit: Stephencdickson
Thalidomide and Congenital Mutations
In the 1960s, two medical professionals; Dr Widukind Lenze and Dr William McBride, observed an association between the use of thalidomide in expecting mothers and congenital malformations.
Once publicized, these findings were further backed by several cases across the globe with a reported 10,000 children thought to have been born with phocomelia.
As a consequence, thalidomide was removed from the market in the majority of countries in 1961, with some still offering the drugs several years after.
Across the cases of patients, a range of abnormalities was noted including:
- Phocoemelia - a congenital deformity whereby the hands and feet are bound to the child’s trunk, absent or grossly underdeveloped;
- Disfigurements of the ear;
- Ocular abnormalities;
- Facial palsies;
- Internal organ damage;
- Congenital heart disease.
In addition to these abnormalities, there was an increase in the number of miscarriages reported by women during the same period of time.
Due to the fact the U.S Food and Drug Administration didn’t approve or license the use of thalidomide, no congenital disabilities were reported in America.
Frances Kelsey was credited for avoiding the tragedy as she was worried about the implications the drug would have on pregnant women and the overall safety of the drug due to incidences of peripheral neuropathy.
In response to the thalidomide tragedy, the pharmaceutical industry has taken great strides to increase the rigor of testing before introducing any new drugs onto the market. Specifically, a set of requirements were introduced for all drug testing to investigate potential developmental toxicity.
The Thalidomide Tragedy | RMIT University
Contemporary Uses of Thalidomide
Since the tragedy, there’s been an increased body of research investigating the action of thalidomide. It was found that thalidomide acts through two main types of mechanisms; anti-angiogenesis and anti-inflammatory. These properties have made the drug an ideal treatment option for a range of medical conditions.
Thalidomide as a Treatment for Multiple Myeloma
Back in 2006, thalidomide became one of the first new agents in over ten years to be approved to treat plasma cell myeloma, a type of bone marrow cancer. Due to boasting anti-angiogenic properties, thalidomide prevents the metastasis, growth, and hypervascularity of cancer tumors.
Thalidomide as a Treatment for Leprosy
Soon after its withdrawal, thalidomide was prescribed to treat a specific implication of leprosy: erythema nodosum leprosum (ENL). ENL is an immunological implication thought to occur in approximately half of those with lepromatous leprosy.
It is characterized by the presence of a range of conditions including neuritis, orchitis, lymphadenitis, and eye inflammation. As ENL is an inflammatory condition, thalidomide’s anti-inflammatory properties make it a viable treatment option.
A lot has been learned, and changes have been made since the thalidomide tragedy. The drug is no longer recommended for use in pregnant women.
However, due to more in-depth research and increased knowledge surrounding the drug’s mechanisms of action, it is now being used to treat and manage a range of health conditions safely.
Sources
- Rehman W., Arfons L. M., & Lazarus H. M. (2011). The Rise, Fall and Subsequent Triumph of Thalidomide: Lessons Learned in Drug Development. Therapeutic Advances in Hematology. DOI: 10.1177/2040620711413165, https://www.ncbi.nlm.nih.gov/pubmed/23556097
- Kim J. H., & Scialli A. R. (2011). Thalidomide: The Tragedy of Birth Defects and the Effective Treatment of Disease. Toxicological Sciences. DOI: https://doi.org/10.1093/toxsci/kfr088
- Vargesson N. (2015). Thalidomide-induced teratogenesis: History and mechanisms. Birth Defects Research. DOI: 10.1002/bdrc.21096, https://www.ncbi.nlm.nih.gov/pubmed/26043938
- World Health Organization. Use of thalidomide in leprosy. https://www.who.int/
- Negera E., Walker S. L., Girma S., et al. (2017). Clinico-pathological features of erythema nodosum leprosum: A case-control study at ALERT hospital, Ethiopia. PLOS. DOI: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5656324/
Further Reading
Last Updated: Mar 15, 2023