Juvenile polyposis syndrome is a condition transmitted from parents to offspring, which causes the development of juvenile polyps inside the large intestine, stomach, or throughout the gastrointestinal tract. These polyps are formed by abnormal collections of cells and tissues which are normally present in the digestive tract, and are therefore considered to be hamartomatous growths. They are invariably benign at first, but have a high risk of malignant change.
The number of polyps that develop over one’s lifetime may vary from four or five to hundreds. The site of polyp formation varies with the type of syndrome. T here are three types:
- Juvenile polyposis of infancy
- Juvenile polyposis, generalized
- Juvenile polyposis coli
In the first type, polyps are present in the whole of the gastrointestinal tract from infancy. In the second and third forms, polyps develop either throughout the whole digestive tract (generalized form) or only in the colon. Their appearance starts in childhood. The infantile form has the worst prognosis and is the most difficult to treat.
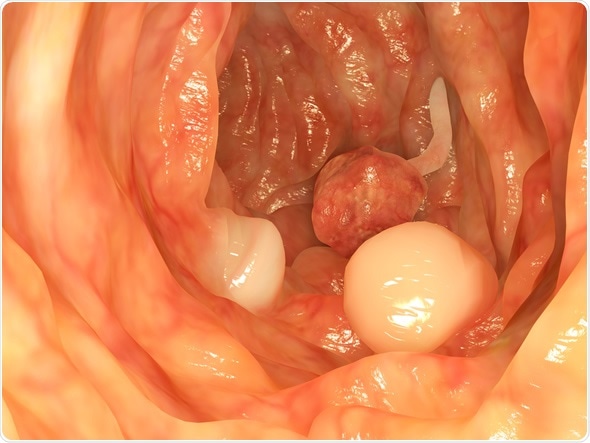
Intestinal polyps - Image Copyright: Juan Gaertner / Shutterstock
Complications
Adenomatous change of the juvenile polyps may occur, with subsequent cancerous transformation in approximately 40% of cases. Large polyps may cause bowel intussusception or obstruction. Polyps may bleed into the intestine, producing anemia, if prolonged.
Treatment
The main aim of treating the juvenile polyposis syndrome is to prevent the development of malignant tumors from any of the polyps, and to prevent complications due to an excessively large polyp. The greater the number of polyps, and the earlier they develop, the higher is the chance of cancerous transformation. Any polyp may be the site of cancerous tumor. Treatment is focused on polyp removal before malignancy develops. Colorectal cancer is the most common, but malignancies of the stomach, pancreas, and the upper gastrointestinal tract also occur at a higher rate. For this reason, yearly screening of individuals who have juvenile polyps is recommended, via endoscopy of the upper and lower digestive tract followed by biopsy and cytologic examination. 21% of patients with gastric polyps may develop gastric cancer during their lifetime, compared to between 9 and 50% of patients from families with a history of juvenile polyposis syndrome.
Large polyps which are likely to lead to the problems cited above are also targets of removal.
Diagnostic endoscopy in juvenile polyposis consists of a colonoscopy to visualize the extent and number of polyps, as well as removal of a tissue sample for histologic examination and pathologic diagnosis. Treatment is also carried out the same way, by endoscopic removal of polyps from the gastrointestinal tract. The base or pedicle of the polyp is ligated by an endoscopic suture or snare, following which the growth can be cut off without fear of hemorrhage. The procedure is painless.
Screening for juvenile polyposis syndrome
Patients at risk for juvenile polyposis syndrome may be those with:
- A positive family history of polyposis, colorectal cancer, or congenital anomalies associated with this syndrome. These include:
- Hydrocephalus
- Anomalies of the heart
- Intestinal malrotation
- Mesenteric lymphangioma
- Arteriovenous malformation of the lungs
- Meckel diverticulum
- A history of bleeding from the rectum, or of changes in the bowel movement (constipation or diarrhea), abdominal pain, or anemia.
In high-risk patients, the following tests are suggested:
- A complete blood count
- A colonoscopy
- An upper endoscopy
These are usually commenced at the age of 15 years, but should be started earlier in symptomatic patients. Even if the tests are normal, repeat screening is advised every three years.
Yearly screening is recommended if juvenile polyps are detected. All polyps that are detected should be removed. Once no more polyps are found on the annual screening, the frequency may be shifted back to every three years.
Siblings of such patients should be advised to undergo screening and genetic testing if indicated. A family tree is often constructed for such patients, to trace the type of cancer, if any, incidence, age of onset and other relatives affected. Earlier genetic testing is also recommended if the family is positive for a known pathogenic variant of the SMAD4 gene, or shows features of combined juvenile polyposis syndrome-hereditary hemorrhagic telangiectasia (JPS-HHT). Such patients need early screening because the potential complications of HHT may occur even in the first decade of life.
If malignant polyps are detected, a colectomy (removal of a part of the colon) or gastrectomy (removal of part of the stomach) is advised. These procedures may also become necessary if there are too many polyps to remove individually, but this is relatively rare. Following these operations, yearly screening is mandated, until no polyps are detected. Following this, screening every three years is resumed.
References
- http://www.chop.edu/conditions-diseases/juvenile-polyposis-syndrome#.V_PNZPl97V0
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3492476/
- ,https://radiopaedia.org/articles/juvenile-polyposis-syndrome
- https://www.insight-group.org/syndromes/juvenile-polyposis/
- https://www.omicsgroup.org/
- https://www.ncbi.nlm.nih.gov/books/NBK1469/
- https://entsoc.org/
Further Reading
Last Updated: Jan 2, 2023