Skip to:
Coronary arteries are the blood vessels which are involved in the supply of oxygen-rich blood to the heart. In some cases, the coronary arteries may become narrow and hardened due to accumulation of plaque in the blood vessels.
Cholesterol plaque in artery with human heart anatomy. Image Credit: Explode / Shutterstock
The condition, known as atherosclerosis, can lead to blockage of blood flow and cause devastating consequences such as coronary heart disease. Medications may help to restore the normal blood supply to the heart; however, in severe cases, where medication is ineffective, coronary angioplasty may be required.
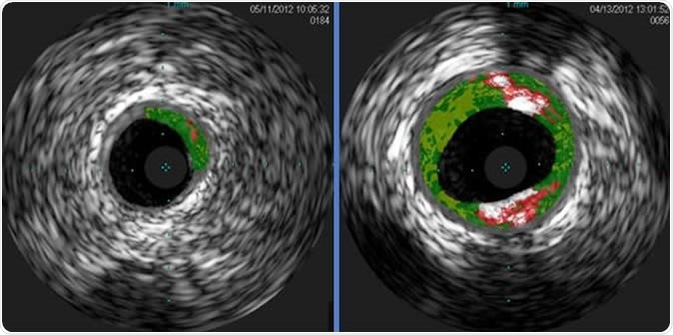
Shown are cross-sectional ultrasound images of coronary arteries from patients enrolled in a study. Plaque buildup (colored areas) in an artery from a patient that lacks sensitivity to red meat allergen (left) is much lower than plaque levels in an artery from a patient with sensitivity to red meat allergen (right). Courtesy of Angela Taylor, M.D., University of Virginia Health System
What is a coronary angioplasty?
A coronary angioplasty is a surgical procedure used to widen a blocked coronary artery. The procedure usually involves the use of a device with a small balloon to widen the blocked blood vessel; however, nowadays the procedure is performed by inserting a tiny tube-like structure, called a stent, into the blocked coronary artery.
The stent acts like a scaffold and helps to open the narrowed coronary arteries. Stents thus allow adequate blood supply to the heart and are left in place indefinitely. Stents are also used to treat aneurysm (outward bulging) of the aorta. The aorta, the body’s largest artery, carries oxygenated blood from the left side of the heart to the rest of the body.
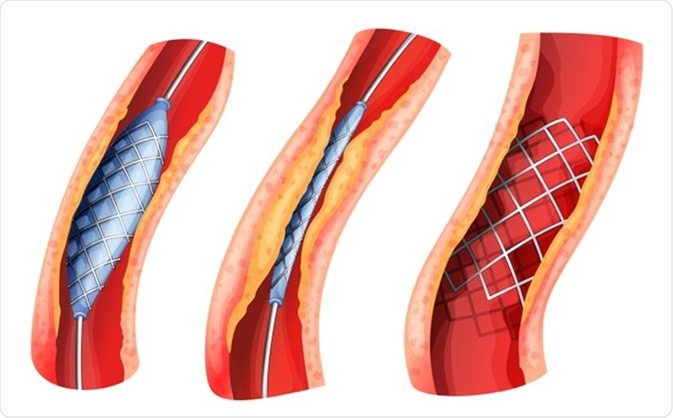
Illustration of a stent used to open blocked artery Image Credit: BlueRingMedia / Shutterstock
What are the types of stent?
Currently, two main types of stent are available - bare metal stent and drug-eluting stent.
Bare metal stent – Bare metal stents were developed in the mid-1990s; however, it was observed that using bare metal stents, in some cases, causes the arteries to narrow again. This phenomenon was observed because the body’s immune system considers the stent as a foreign object. The immune attack leads to inflammation and growth of abnormal tissues nearby the stent. This drawback has however been solved with the advent of drug-eluting stents.
![Mick Hensman [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)] Mick Hensman [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]](https://www.news-medical.net/image-handler/picture/2019/9/%40bare_metal_stentj.jpg)
Mick Hensman [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
Drug-eluting stent – The drug-eluting type is coated with medications that decrease the body’s immune response to stent; the medications also reduce the growth of abnormal tissues around the stent.
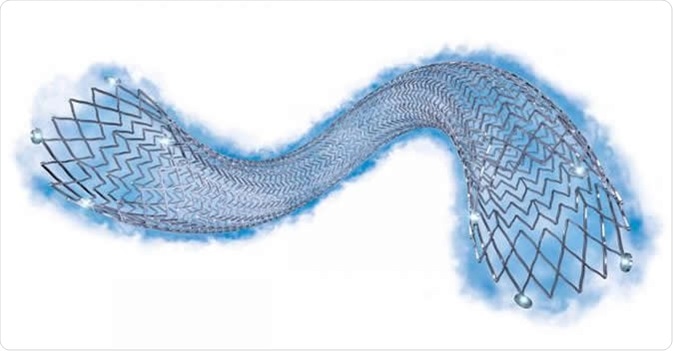
Eluvia™ is a drug-eluting vascular stent system for clinical treatment of peripheral artery disease (PAD). Image Credit: Boston Scientific
The use of drug-eluting stent is associated with delayed healing of the target coronary artery; hence, patients are prescribed anticoagulants for almost a year after the procedure.
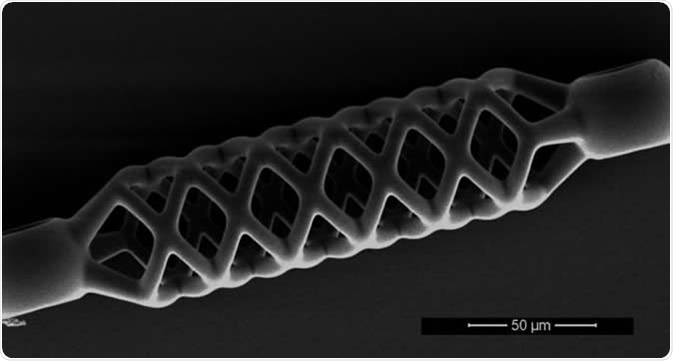
This microstent is just 50 micrometers (0.05 mm) wide and half a millimeter long. Image Credit: De Marco et al, Adv Mater. Techn. 2019; ETH Zurich
The use of blood thinning agents or anticoagulants also reduces the risk of development of blood clots, which may block the stent and cause heart attacks.
Bare-Metal, Drug-Eluting, and Bioresorbable Stents in Context
What are the complications from a stent?
Even though stents are generally safe to use, sometimes complications may occur during and after the stenting procedure. Complications are usually observed in people who have had previous surgeries to treat blocked arteries or who are affected with chronic diseases such as heart failure, kidney disease, or diabetes.
The following complications may be observed:
Reactions to the dye used in the procedure - In some cases, an allergic reaction may occur to the dye used to show the blood vessels by X-ray. In rare cases, the contrast dye may cause kidney damage.
Complication associated with catheters used - Complications such as bleeding or discomfort can also arise during insertion of catheter. The nearby blood vessels may also get damaged due to the catheter.
Blood clotting - A blood clot is the most serious complication that can occur within the stent. Blood clots can lead to severe complications such as heart attack, stroke, and thromboembolism to another part of the body.
Chest pain – Chest pain is a symptom of re-stenosis. Re-stenosis is the re-narrowing of the artery where a stent was placed. Re-stenosis is caused by abnormal tissue growth within the target artery. Treatment of re-stenosis involves both angioplasty and use of another stent, typically a drug-eluting stent.
Stent or stent graft failure - Occasionally stent grafts which are used to treat aortic aneurysm may move from its placed position. This may cause the stent to break within a peripheral artery and lead to blood leakage out of the graft. In such conditions, the person affected may experience symptoms similar to those experienced before getting a stent; however in some cases it may be asymptomatic. Physicians usually use imaging techniques such as computed tomography angiography (CT) or ultrasound to monitor the stent graft and diagnose such complications.
Arrhythmia or an irregular heartbeat and infection are some other risks associated with the use of stents.
British Heart Foundation - Your guide to Angioplasty and Stents
Living with stents
While living with stents, it’s important for the patient to be well informed of the possible risks and complications that are specific to the stent used in the body. It is important to follow the assigned treatment plan, opting for healthy lifestyle choices, and getting regular medical check-ups. Lifestyle changes which may help include
- Weight reduction, if indicate
- Regular exercise
- Eating a diet rich in fruits and vegetables
- Managing stress and quitting smoking
Further Reading
Last Updated: Sep 18, 2019