Cervical spondylosis is caused by abnormal wear on the bones that make up the spine (vertebrae) in the neck region.
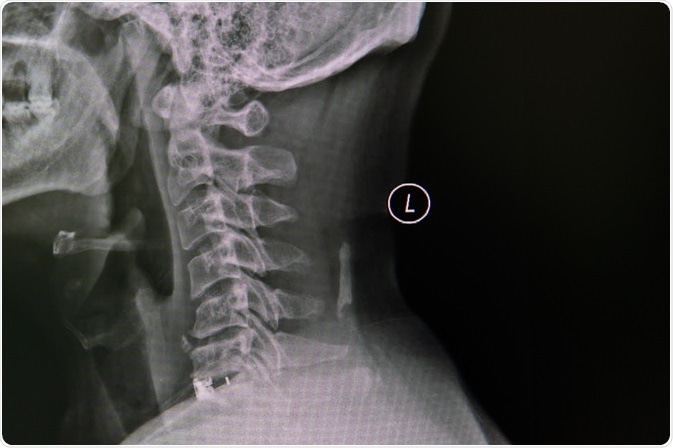
Image Credit: Nuiza11/Shutterstock.com
Not only is it common, but it is also a frequent cause of neck pain. It is related to aging as well as to degenerative changes of the strong tough cartilage that cushions the separate bones that make up the cervical spine. Sometimes, in addition to age- and wear-related factors, there may be bone anomalies, such as bone spurs or growths which aggravate the damage.
As the cartilage breaks down and becomes more fragile, the vertebrae settle down on each other, reducing the space between them. As a result, there is abnormal pressure on the nerve bundles (nerve roots) that leave the spinal cord at each of these spaces, to form the major nerves that supply various parts of the body, and a few fibers to the lower limbs as well.
As a result, the individual experiences pain, tingling, numbness, and weakness in the arms. Chronic neck pain is a constant feature, felt over the shoulder blade. It could spread to the upper arm and downwards, though finger involvement is rare, but not unknown. Headaches are also common.
Treatment overview
There are different ways of managing chronic neck pain due to cervical spondylosis. One way is physical therapy. Neck traction may also be used to relieve the pressure. Massage is another option, as is spinal manipulation. Acute pain may require cold or hot packs.
The mental distress caused by cervical spondylosis may be helped by cognitive behavioral therapy, which is a form of talk therapy, or counseling, aimed at helping to understand what causes the pain and how you can continue to be productive with this condition.
Medication is commonly used, including non-steroidal anti-inflammatory drugs (NSAIDs) are used over the long term. Anti-seizure medications that also inhibit pain pathways are sometimes used to reduce the pain when the nerve damage is severe at the time of the initial presentation.
Antidepressants are useful to combat the pain and lift the mood in patients with cervical spondylosis. For very severe pain, opioids may be prescribed. Muscle relaxants are also prescribed to relieve muscle spasms in the neck muscle, brought on by irritation of the nerve roots. However, opioids and muscle relaxants can also cause drug dependence and should be avoided in favor of alternative therapies when available.
Surgical management is typically a last resort, when pain persists to a severe degree despite these treatments, or if weakness or paralysis sets in, indicating pressure on the spinal cord.
Medications
NSAIDs
NSAIDs act by inhibiting two cyclo-oxygenase enzymes (COX1 and COX2), to prevent further activation of the inflammatory pathway by this mechanism. They have not been subjected to clinical trials in the treatment of cervical spondylosis but are the most commonly used drugs in this condition.
They are preferred by most practitioners because of their pain-relieving and anti-inflammatory action, which will hopefully reduce swelling and pressure around the affected nerve, making it less susceptible to compression and damage.
Direct comparisons of NSAID efficacy to a pure analgesic like acetaminophen have not been performed. They are more effective than placebo, in the treatment of other joint inflammations. The widespread occurrence of COX1 and COX2 in the body accounts for their many side-effects.
Opioids
Opioids act to relieve pain by a central action, that is, by binding to receptors on nerve cells in the pain pathways within the spinal cord. This binding inhibits the further release of neurotransmitters, chemicals that pass on the nerve signaling along that pathway. They also activate midbrain neurons to inhibit pain sensation.
They are addictive and may not be effective in the pain of nervous origin over the long-term, as continuing opioid stimulation changes neurotransmitter levels, leading to tolerance. Also, they do not seem to improve employment chances or social functioning in patients. However, they can reduce pain to acceptable levels in many patients without producing addiction.
Muscle relaxants
Muscle relaxants act by relieving the spasm of the neck muscles and produce sedation which promotes better sleep. The greatest benefits are experienced in the first week of taking these drugs, and they are also known to be habit-forming. As a result, they should not be prescribed for over 2 weeks and should be tapered quickly within this period.
Antidepressants
Antidepressants are widely used for their effect on pain, though modest and not linked to improved function. Tricyclic antidepressants are generally not suitable for older patients due to the risk of sedation, cardiac toxicity and drop in blood pressure in some situations.
Antiepileptics
Antiseizure drugs used in cervical spondylosis are the main antagonists of GABA receptors and be not of benefit in neuropathic pain as in this condition.
Steroids
Corticosteroids are biological molecules that are very powerful anti-inflammatory and immunosuppressive agents. Like NSAIDs, there is not much rigorous evidence to support their effectiveness in this condition. They should be used in selected patients only, for short periods up to 3 days at the full dosage and then tapered over the next 7-10 days. Cervical epidural steroid administration may perhaps more useful in symptomatic relief but is also riskier. Its value remains to be proved, as indeed that of systemic steroids.
Sometimes steroids are injected into the epidural area, around the spinal cord, but such injections are not recommended frequently, nor do they produce lasting relief.
Physical therapy
Many trials of physical therapy offered in a structured way have shown that there is an early improvement in pain severity, better muscle strength, and better maintenance of sensation. However, at one year the difference in objective clinical signs or patient satisfaction is nil. Physical therapy consists of different types of isometric exercises to stretch and relax the muscles, manual therapy like spinal manipulation and massage.
Hot fomentation helps relieve the pain over the short-term, though the lasting benefit is absent. Ultrasound does not show any evidence of efficacy. Wearing a neck brace or a soft neck collar may also help the muscles to rest, but if worn too long it can cause muscle weakening.
Alternative and complementary medicine
Traditional Chinese medicine, acupuncture, and reflexology are among commonly offered alternative and complementary treatments for cervical spondylosis. Acupuncture seems to give short-term relief of pain but no functional improvement.
Surgical management
Surgery is reserved for patients who do not respond to three or more months of conservative treatment. Different types of surgery may be carried out depending on the patient.
Some procedures that are commonly recommended include discectomy (removal of a weakened bulging intervertebral cartilage or “disc” to relieve its pressure on the nerve roots near it); removal of various parts of the affected vertebra such as laminectomy and corpectomy; and spinal fusion to stabilize the spine. However, there is no evidence that surgery positively affects long-term outcomes.
Sources
Medlineplus.gov. (2019). Cervical spondylosis. https://medlineplus.gov/ency/article/000436.htm
Mayoclinic.org. Cervical spondylosis. www.mayoclinic.org/.../drc-20370792
Loris A. Chahl. Opioids - mechanisms of action. Australian Prescriber 1996;19:63-5. DOI: 10.18773/austprescr.1996.063. www.nps.org.au/.../opioids-mechanisms-of-action
Nonoperative modalities to treat symptomatic cervical spondylosis. Kieran Michael Hirpara, Joseph S. Butler, Roisin T. Dolan, John M. O'Byrne, and Ashley R. Poynton. Advances in Orthopedics, 2011, 2012; 2012: 294857. https://dx.doi.org/10.1155%2F2012%2F294857. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3168941/
State of the art in degenerative cervical myelopathy: an update on current clinical evidence. Jefferson R. Wilson, Lindsay A. Tetreault, Jun Kim, Mohammed F. Shamji, James S. Harrop, Thomas Mroz, Samuel Cho, and Michael G. Fehlings. Neurosurgery, volume 80, issue 3S, March 2017, pages S33–S45, https://doi.org/10.1093/neuros/nyw083. https://academic.oup.com/neurosurgery/article/80/3S/S33/3045012
Surgery for cervical radiculopathy or myelopathy. Nikolaidis I., Fouyas I. P., Sandercock P. A., Statham P. F. and Lynch C. Cochrane Database Systematic Review, 2010 Jan 20;(1): CD001466. DOI: 10.1002/14651858.CD001466.pub3. https://www.ncbi.nlm.nih.gov/pubmed/20091520
Last Updated: Jan 23, 2020