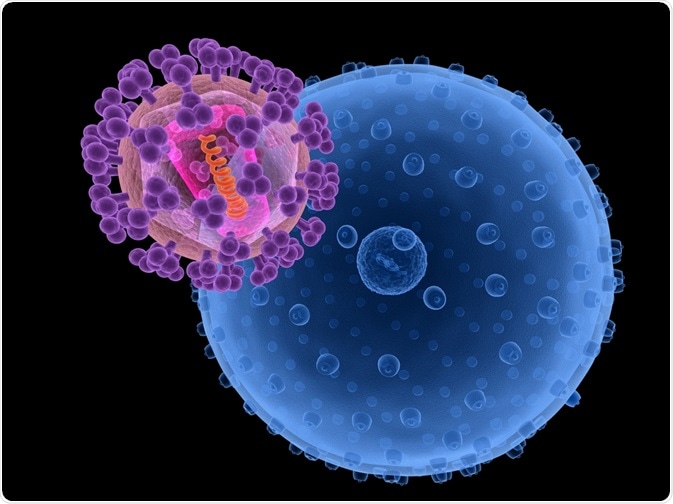
Research on therapies against the Human Immunodeficiency Virus (HIV) has repeatedly demonstrated the potential of broadly neutralizing antibodies (bn-Abs) as successful therapeutic agents. Injection of such antibodies leads to a decrease in viral concentrations in blood. However, repeated injections are necessary to prevent the recovery of the virus.
In this case study, researchers from the United States of America carried out a proof-of-concept experiment which showed that gene therapy could be used to stimulate bn-Abs long-term in monkeys. However, while this caused the viral load in the blood to drop significantly, so did the levels of antibodies, as they were being cleared by the immune system.
 Sebastian Kaulitzki | Shutterstock
Sebastian Kaulitzki | Shutterstock
Developing efficacious antibodies against HIV
There is currently no effective cure for HIV, although drugs that maintain the viral load of HIV at a low level have been developed. However, the quality of life of HIV patients remains impaired since the virus stays in their bodies, carrying the risk of transmission of the virus via body fluids.
Research remains active in searching for effective treatments, but the virus evolves at a high rate and escapes the immune system by hiding as silent pro-virus in cells. Another difficulty arises since the virus retains its host cell’s membrane, thus limiting the possibilities of the immune system to identify HIV as a foreign invader.
However, in some cases broadly neutralizing antibodies (bn-Abs) from HIV infected patients have been identified which target HIV-specific proteins that protrude out of the membrane envelope.
Once bn-Abs have been identified, they can be produced biotechnologically and be administered by injection to HIV infected people. Unfortunately, to manage the concentration of HIV virus circulating in body fluids, recurrent injections of bn-Abs are needed, since the viral concentration can easily recover once antibody levels diminish.
Continuously elevated antibody concentrations are therefore a desirable target for the treatment and prevention of HIV.
Adenovirus-mediated gene therapy for HIV
The scientists investigated Rhesus macaque monkeys infected with the simian/human immunodeficiency virus (SHIV-AD8), which is related with HIV, but infects the monkeys. Gene transfections in monkey tissues were achieved with adenovirus vectors, which are commonly used for cell transfections as they do not cause any notable diseases.
These adenoviruses carried the information for bn-Ab sequences which had been optimized in sequence to be similar to typical Rhesus macaque antibodies, which have characteristic sequence differences compared with human antibodies.
The monkeys received intramuscular adenovirus injections, since the scientists were aware that transfected skeletal (i.e. muscular) cells had been shown to express genes received by transfection over extended periods of several years.
After the injection of the gene therapy agent, the scientists monitored the concentration of SHIV in the blood of the monkeys along with the concentrations of the different antibodies.
 Kateryna Kon | Shutterstock
Kateryna Kon | Shutterstock
The gene therapy was effective, but only in a small number of monkeys
The scientists observed in three of the monkeys a strong suppression of the SHIV concentration in blood. Simultaneously, they observed an elevated concentration of the antibodies delivered by the gene therapy agent.
However, in another 12 monkeys, the gene therapy did not lead to a long-term suppression of the SHIV, and the bn-Ab concentrations remained low. In addition, for the three monkeys where the gene therapy had shown an effect, the SHIV could still be recovered from blood samples, which means that the infection had not been completely eradicated.
The researchers highlighted that these were promising proof-of-concept results, which however require further research. As a major challenge, the investigators observed that the bn-Abs were recognized as foreign agent by the monkeys’ immune system which in turn attacked and neutralized the bn-Abs. They associated this with the fact that the bn-Ab sequences were in a “mature” state.
When a foreign antigen is detected by the immune system, early antibodies against the antigen first occur that are “immature” and “close to the germline”. The antibody is then tested and mutated in multiple selection cycles until a “mature”, often more effective antibody state is reached.
When given as a therapy, these “mature” antibodies are more likely to be attacked by the immune system. While this poses an additional challenge, research on other antibodies from a vaccination trial has recently shown that early antibodies that are indeed “closer to the germline” can be isolated by efficient screening methods.
While a cure to HIV is thus still not reached, the adenoviral gene therapy promises a path to improve the management of HIV infections by keeping the viral concentrations low, thus managing disease symptoms. Further research will however be required to improve the therapy effectiveness.
Sources
- Martinez-Navio JM et al., Adeno-Associated Virus Delivery of Anti-HIV Monoclonal Antibodies Can Drive Long-Term Virologic Suppression. Immunity 2019, 50, 567-575; DOI: 10.1016/j.immuni.2019.02.005.
- Ecker DM et al., The therapeutic monoclonal antibody market. MAbs 2015, 7 (1), 9-14; DOI: 10.4161/19420862.2015.989042.
- Ganser-Pornillos B et al., The Structural Biology of HIV Assembly. Curr Opin Struct Biol 2008, 18 (2), 203-217; DOI 10.1016/j.sbi.2008.02.001.
- Rijal P et al., Therapeutic Monoclonal Antibodies for Ebola Virus Infection Derived from Vaccinated Humans. Cell Reports 2019, 27, 172-186; DOI: 10.1016/j.celrep.2019.03.02.
Further Reading
Last Updated: Aug 26, 2019