Immunoglobulins are antibodies which are encoded for by large multigene families. Immunoglobulins are shaped by the process of somatic rearrangement, along with other genetic changes, during the initial development of B lymphocytes.
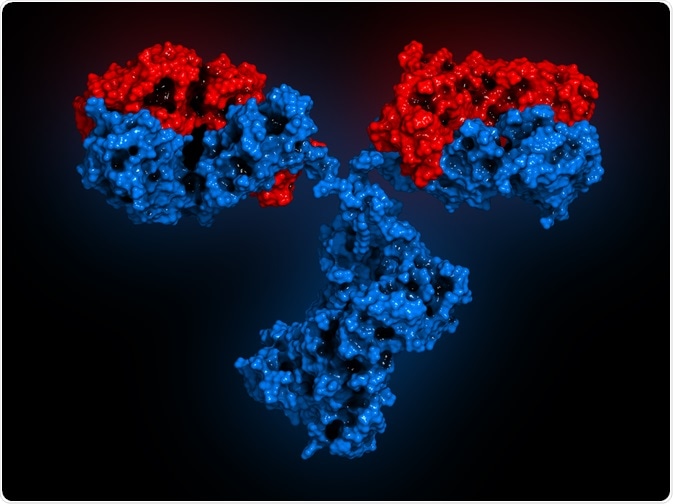 Image Credit: molekuul_be / Shutterstock
Image Credit: molekuul_be / Shutterstock
Immunoglobulins are found inside all vertebrates and act as the initial detector of any foreign bodies that come into contact with the host organisms’ bodily systems, such as pathogenic bacteria, for example.
They also mediate the body’s response to a pathogenic infection by initiating inflammation and opsonizing foreign bodies for a more effective immune response.
IgG is the type of immunoglobulin most commonly found within human serum and can be broken down into four sub-classes: IgG1, IgG2, IgG3, and IgG4.
IgG’s make up 10-20% of human plasma and were discovered in the 1960’s after studies were performed on rabbit antisera against human IgG proteins.
Different subclasses of IgG have approximately 90% similarity with respect to their amino acid structures, but each subclass has unique antigen binding methods, complement activation, immune complex formations, half-life, and trigger their respective effector cells in different ways.
What does each IgG subclass do?
IgG1 antibodies
IgG1 antibodies are produced when an organism experiences an anaphylactic or allergic reaction to a substance, along with IgE.
The production of IgG1 has mainly been observed to induce essential cardio-pulmonary responses to anaphylaxis, with these responses mainly being mediated by the ‘Fc’ region of the IgG1 antibody.
IgG2 antibodies
IgG2 antibodies are usually found in relation with the host reaction to bacterial capsular polysaccharide antigens, with IgG2 deficiency being associated with an increased susceptibility to certain bacterial infections.
During the course of infection, when certain released cytokines induce the expansion of B-cell clones within the human immune system, the pre-committed B-cells have been shown to induce the secretion of IgG2 in vitro.
IgG3 antibodies
IgG3 antibodies are mostly found to be associated with effector responses to foreign antigens. They are also produced when the human body becomes infected with a parasite.
For example, during a cross-sectional survey carried out in Western Africa in 1998, 178 individuals aged between 1-75 years were vaccinated against Plasmodium falciparum – a type of malaria – and their antibody responses assessed.
It was observed that in the individuals aged 10 years or above, the specific antibodies that were produced were mostly IgG3.
It has therefore been hypothesized that the age- or exposure-related acquisition of IgG3 antibodies might play a role in the development of clinically protective immunity to the Plasmodium parasite.
IgG4 antibodies
The final immunoglobulin subclass IgG4 is commonly associated with chronic exposure to an antigen, as in immunotherapy, and with filarial or helmintic infection. IgG4 has also been associated with several autoimmune diseases, including asthma, pancreatitis, and certain allergies.
IgG4 is therefore used as a biological marker for many diseases, as significantly higher levels are indicative of an immune response. For example, higher than average volumes of IgG4 in the blood and pancreatic tissue can facilitate the diagnosis of autoimmune pancreatitis.
The IgG4 antibody has a similar physical structure and half-life to IgG2 – with both of these IgG subclasses being seen in conjunction with IgE (immunoglobulin E), which activates mast cell degranulation, usually resulting in allergies and/or asthma.
Conclusion
IgG comes in many different subclasses – most of which have inherently different functions from one another, but are all an integral part of the body’s immune system.
Most of the time, the actions of these immunoglobulins are useful, but they can sometimes become over-active and cause autoimmune diseases, which are typically difficult to treat, and usually have no direct cure.
Learning more about the different IgG subclasses could be a means to discovering new clinical treatments and cures for a range of autoimmune disorders, as well as developing methods to make the host immune system more efficient in a given organism – thus reducing the need for current clinical treatments, such as antibiotics.
Further Reading
Last Updated: Jul 20, 2023