In a recent study published in the journal Nature Immunology, researchers conducted a large-scale phenotyping examination of patients with long coronavirus disease 2019 (long COVID, LC) after hospitalization to investigate underlying inflammatory mechanisms.
LC is a severe type of COVID-19 that affects millions of individuals globally. Despite recent variations, LC remains prevalent and likely to create long-term health problems. Sustained inflammation has been documented among adult LC patients, although investigations are limited in scale, duration, and immune mediators examined. The post-hospitalization COVID-19 (PHOSP-COVID) trial in the United Kingdom found inflammatory profiles among 626 individuals with health impairments following COVID-19, with higher interleukin-6 (IL-6) expression and mucosal inflammation among individuals with severe impairments. LC complexity and disease burden warrant identifying underlying inflammatory pathways to develop effective therapeutics and improve the standard of care.
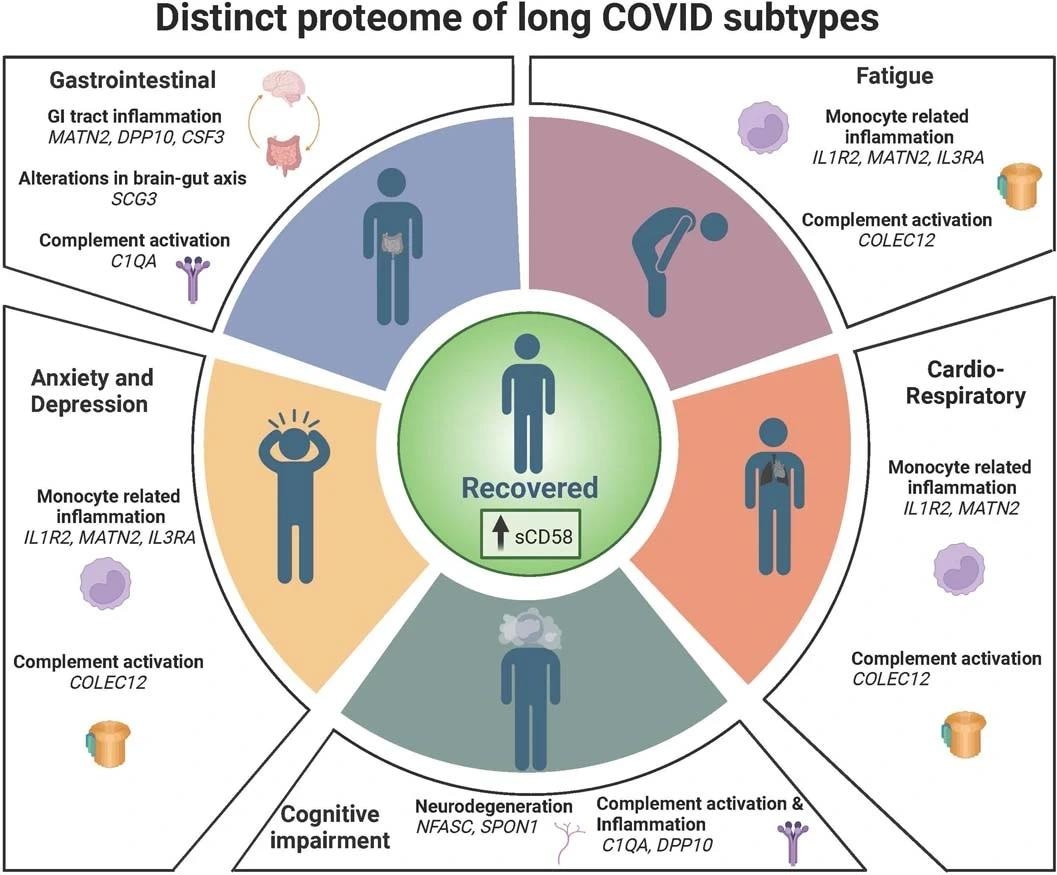
Summary of interpretation of key findings from Olink measured proteins and their association with CardioResp (n = 398), Fatigue (n = 342), Anx/Dep (n = 219), GI (n = 134), and Cognitive (n = 65) groups relative to Recovered (n = 233). Letter: Large-scale phenotyping of patients with long COVID post-hospitalization reveals mechanistic subtypes of disease
About the study
In the present study, researchers explored the inflammatory pathways underlying LC symptoms.
The researchers examined adult PHOSP-COVID trial participants who had a prognosis of fewer than six months following COVID-19 hospitalization. They gathered data from February 2020 to January 2021, using the International Severe Acute Respiratory and Emerging Infection Consortium World Health Organization Clinical Characterisation Protocol United Kingdom (ISARIC4C study), hospital records, and self-reporting to account for variables influencing symptom outcome.
The team examined 368 plasma proteins in 657 subjects after hospitalization for at least three months (median, 6.10 months). They confirmed COVID-19 clinically or by polymerase chain reaction (PCR) and assessed its severity using World Health Organization (WHO) ratings. They classified patients based on symptom type, including cardiorespiratory, fatigue, emotional, anxiety/depression, gastrointestinal, and cognitive symptoms. They used multivariable penalized logistic regressions (PLR) to conduct their analysis. To confirm the study findings, the researchers conducted chemiluminescent immunoassays on serum obtained from 58 subjects and re-analyzed data using LC criteria given by the National Institute for Health and Care Excellence (NICE) and the Centers for Disease Control and Prevention (CDC). They also conducted a network analysis of PLR-highlighted immunological mediators within each LC group to investigate their relationships with LC symptoms.
Furthermore, the researchers investigated hormonal variations between male and female LC patients. They also investigated whether local respiratory tract inflammation remained after COVID-19 and whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) persistence may explain the inflammatory profiles observed in the cardiorespiratory group. They monitored SARS-CoV-2-specific antibody titers among unvaccinated individuals, including 19 recovered individuals and 35 LC patients.
Results
The study examined the severity of COVID-19 in patients aged 55–57 years, categorizing them as WHO 3–4 (no oxygen assistance), WHO 5–6 (oxygen support), and WHO 7-9 (critical care). Among 657 subjects profiled ≥3 months after hospitalization, 426 showed one or more LC symptoms, whereas 233 had recovered. LC was associated with enhanced myeloid inflammatory and complement activational markers, with interleukin-1 receptor, type II (IL-1R2), matriline-2 (MATN2), collectin-12 (COLEC12), and protocadherin-1 (PCDH1) associated with cardiopulmonary symptoms, anxiety/depression, fatigue, colony-stimulating factor 3 (CSF3), isthmin (ISM), and MATN2 elevated among individuals with gastrointestinal symptoms, and complement C1q A (C1QA) among cognitively impaired LC patients.
Additional biomarkers of neural tissue repair changes, including neurofascin (NFASC) and spondin-1 (SPON-1), were higher among cognitively impaired LC patients, whereas secretogranin III (SCG3), indicating gut-brain axis disruption, was increased among those presenting with gastrointestinal complaints. Gastrointestinal symptoms may be caused by enteric inflammation since the GI group has higher dipeptidyl peptidase 10 (DPP10) expression than recovered patients.
Elevated fibrinogen levels in LC patients indicated complement pathway activation, complement dysregulation, and thrombosis as risk factors for severe COVID-19. Elevated lymphocyte-function antigen 3 (LFA-3) was related to a decreased risk of LC symptoms, especially cardiorespiratory symptoms, tiredness, and anxiety/depression. These symptoms were associated with lower IL-2 levels. The study findings indicate that reducing myeloid inflammation and improving tissue regeneration are connected with recovery, supporting immunomodulatory drug use in clinical studies.
In women aged 50 and up, inflammatory markers were considerably higher in the cardiorespiratory and exhaustion groups, whereas CSF3 was higher in the gastrointestinal group. Several inflammatory markers [C-X-C motif chemokine ligand 10 (CXCL10), CXCL11, tumor necrosis factor (TNF), vascular endothelial growth factor (VEGF), trefoil factor 2 (TFF2), and IL-1α] elevated in the upper respiratory tract after COVID. However, there was no correlation between plasma and nasal mediator levels, indicating that upper respiratory tract inflammation is not specific to cardiorespiratory symptoms. SARS-CoV-2-targeted immunoglobulin G (IgG) titers remained increased in a few individuals with protracted COVID, although the virus was undetectable in sputum. The inflammatory marker analysis of nasal secretions revealed no correlation with LC symptoms.
The study found indicators of myeloid inflammation and complement activation in LC patients six months following hospitalization. The findings indicate that researchers consider LC subphenotypes in managing the condition and antiviral or immunomodulatory drug use in controlled trials. The study highlighted unique inflammatory pathways linked to tissue injury in LC subtypes, which future trials may assess.