Following the publication of the genetic sequence of the severe acute respiratory syndrome virus 2 (SARS-CoV-2) virus in January 2020, pharmaceutical companies worldwide have been racing to develop a safe and effective vaccine, with many reaching clinical trials in record time.
The method of action and constituents of any particular vaccine may vary wildly, just as the viruses they protect against target different cells and take different routes to infection.
 Image Credit: Viacheslav Lopatin / Shutterstock.com
Image Credit: Viacheslav Lopatin / Shutterstock.com
SARS-CoV-2 has been well reported to induce a range of immune responses in patients, with some remaining non-symptomatic while others just as heavily infected require hospitalization. This variability makes the development of a long-lasting vaccine that will guarantee immunity throughout the whole population highly challenging.
SARS-CoV-2 binds to the angiotensin-converting enzyme 2 (ACE2) receptor, expressed in many tissues and organs throughout the body, particularly in the lungs, gut, and brain. The wide presentation of the ACE2 receptor is partly the reason for the highly variable symptoms of COVID-19.
T-cells are responsible for immune memory, and the generation of high-affinity antibodies and SARS-CoV-2 infected patients tend to show elevated antibody levels for significant periods post-infection.
Unlike most other vaccines that are either inactivated (consist of virus particles that have no disease-producing capacity) or attenuated (made less harmful or virulent), many of the vaccines approved for use against COVID-19 so far are nanotechnology-based.
This article will discuss two of the most prevalent vaccination technologies being used for SARS-CoV-2 and some of the approved vaccines in use these methods.
mRNA vaccines
Two of the earliest companies to announce successful vaccines were Moderna and Pfizer-BioNTech, both of which utilize lipid nanoparticles to encapsulate an mRNA payload. The mRNA encodes for the production of an antigen known to be specific to SARS-CoV-2, allowing the cell's machinery to produce the antigen to which the body will then develop immunity.
The use of a lipid nanoparticle carrier can potentially provide several benefits, including the possibility of direct cytoplasmic delivery and increased specificity towards antigen-presenting cells. The full details of each formulation are yet to be released. However, the Pfizer-BioNTech lipid nanoparticle is known to be slightly cationic, which could potentially aid in cell internalization due to the slight negative charge of the cell membrane.
Both the Moderna and Pfizer-BioNTech vaccines use mRNA that encodes for the spike protein of SARS-CoV-2, which binds with the ACE2 receptor. The spike protein consists of two subunits, the first of which is responsible for the initial binding with ACE2, while the second promotes viral fusion.
The Moderna vaccine, mRNA-1273, specifically encodes for the pre-fusion form of the protein and is largely intact besides two amino-acid substitutions at positions 986 and 987 that help to keep the protein stable in this pre-fusion state. The surrounding lipid nanoparticle is composed of four lipids, the exact structure of which is yet to be announced. However, previously developed lipid-nanoparticle-based vaccines from Moderna contain 1,2-distearoyl-sn-glycero-3-phosphocholine, cholesterol, and polyethylene glycol-lipid, which may also be the case here.
The mRNA utilized by the Pfizer-BioNTech vaccine (BNT162) encodes for the receptor-binding domain of the spike protein only, found on the first subunit of the protein. The mRNA has been modified to incorporate 1-methylpseudouridine, which aids in reducing the immunogenicity of the mRNA and increases translation rate, most likely through improved stability of the molecule, although this has yet to be entirely elucidated.
Again, the exact formulation of the lipid nanoparticle carrier has not been published, though past papers from the company indicate it could contain phosphatidylcholine, cholesterol, and polyethylene glycol-lipid.
mRNA vaccination technology has not yet been approved following initial clinical trials for any other disease. In this case, the comparatively quick development time and urgency of the situation have brought this technology to the fore.
Since the vaccine itself does not carry the antigen, there is little chance of neutralization in the serum, and repeated booster regimens are less prohibitive. Since RNA replicates in the cytoplasm, it does not need to be localized to the nucleus, like DNA.
Concern has been expressed over mRNA vaccines ‘altering your DNA’. However, the mRNA remains in the cytosol after entering a cell and cannot cross the membrane into the nucleus where the DNA is contained. The mRNA degrades quickly in the cytosol. Hence, mRNA vaccines cannot alter DNA.
However, RNA vaccines are a developing technology that are likely to require additional boosts. In light of this, several other companies have instead been working towards a viral vector vaccine.
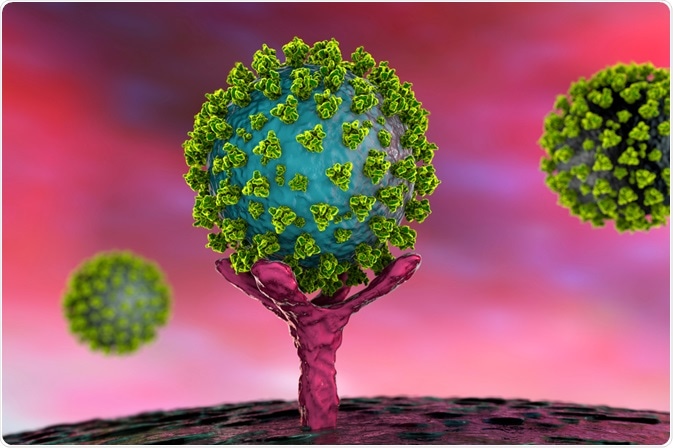 Conceptual illustration of SARS-CoV-2 virus binding to an ACE-2 receptor on a human cell. Image Credit: Kateryna Kon / Shutterstock.com
Conceptual illustration of SARS-CoV-2 virus binding to an ACE-2 receptor on a human cell. Image Credit: Kateryna Kon / Shutterstock.com
Viral vector vaccines
Adenoviruses are simple non-enveloped viruses that contain a linear double-stranded DNA genome and are responsible for a variety of illnesses including cold-like symptoms. Adenovirus vectors are used in vaccines to express foreign antigens and thus stimulate an immune response, achieved by replacing sections of DNA within the adenovirus.
Adenoviral DNA does not integrate into the genome of the host and is not replicated during cell division. Since the adenovirus is sourced from a family of common viruses including the common cold, many patients have already developed neutralizing antibodies, leading to the use of adenoviruses that had originally evolved to infect other species, and to which humans do not have immunity.
The Oxford-AstraZeneca vaccine (ChAdOx1) utilizes an adenovirus vector derived from the chimpanzee, incorporating genetic sequences that instruct cellular machinery to produce the full-length spike protein of SARS-CoV-2. Some changes were made to the genetic sequence that would prevent replication and improve translation, specifically by deleting E1 and E3 and incorporating a tissue plasminogen activator leader sequence.
The Chinese vaccine company CanSino took a similar vector approach, though it uses an adenovirus native to humans often employed as a vaccine vector: adenovirus type 5. The company noted that around half of their early participants had pre-existing immunity towards adenovirus type 5, compared to only 1 in 98 patients for the chimpanzee sourced Oxford-AstraZeneca vaccine.
Both vaccines demonstrated some adverse effects in early clinical trials, including mild to moderate pain, fatigue, and headache. The Oxford-AstraZeneca vaccine was co-administered with the anti-inflammatory drug acetaminophen as a precaution that seemed to lessen these problems.
Meanwhile, the Johnson & Johnson vaccines uses Adenovirus 26 (Ad26), a one dose vaccine that has come out of phase III trials as safe and effective.
Efficacy and comparisons
Dozens of additional companies are working towards creating a safe and reliable vaccine, some utilizing the technologies described above. In contrast, others rely on more classical live-attenuated or inactivated virus vaccine platforms.
These vaccines have not been explained here, but there are benefits and limitations to both. For example, whilst they are well-established technologies, attenuated vaccines may be unsuitable for use in immunocompromised individuals, making them less than ideal for protecting those most vulnerable, and inactivated vaccines often have low immunogenicity, requiring multiple boosters.
Each of the vaccines discussed here has been found to possess acceptable safety profiles across phase I, II, and III clinical trials by various governments and organizations, having now been administered to millions of patients from across the globe. There are several more that have been approved around the world.
Pfizer-BioNTech and Moderna report a high degree of efficacy, stated to be as high as 95% depending on the age group, sex, ethnicity, infection status, and dosing regimen. Pfizer-BioNTech has been approved in several countries and has emergency use approval in many countries around the world including the UK, US, EU and validation for emergency use by the World Health Organization (WHO). Moderna has been approved for use in Switzerland and has emergency use approval for many other nations including the UK, US and EU.
The CanSino one-shot vaccine is approved in China for general use and some other countries for general use, with the company announcing a 65.28 percent efficacy rate for preventing symptomatic COVID-19, although trial details are not yet published.
The Oxford-AstraZeneca vaccine has been approved for general use in Brazil, and for emergency use in several countries including emergency use validation by the World Health Organization (WHO).
In March 2021, some countries in the EU temporarily suspended rollout of the vaccine due to a possible risk of blood clots. The stance of the WHO (as of 18 March) is that the benefits of the vaccine outweigh the risks and that it should continue to be administered, and that safety data will continue to be reviewed and made transparent. Currently, although Denmark has stopped the rollout of the vaccine, the EU has resumed use; however, some countries are restricting its use to older people as the blood clot risk seems to be in younger patients.
The Johnson & Johnson vaccine is a one-shot vaccine now being mass-produced and rolled out across the world. It has been approved for emergency use by several countries including the FDA (US) and EU. This has been stated to be 86% effective at preventing severe COVID-19 and 72% effective at preventing all COVID-19. In April, there was a pause of the vaccine in the US due to an extremely rare risk of blood clots. However, after a review by the FDA and CDC, this pause has now been lifted.
A key point is that it is difficult to compare the efficacies of these vaccines, due to differences in clinical trial designs. Furthermore, earlier clinical trials will not have included exposure to the concerning variants that have appeared since. Most vaccines are now being tested for efficacy against these strains, and some are showing reduced efficacies (although none have yet been shown to be ineffective).
Many of the vaccines are now undergoing further development in order to adapt them to new strains of the virus. Some of the vaccines are undergoing further phase III trials or carrying out further trials on specialized groups such as pregnant women and children.
It is important to have multiple different vaccine approaches to SARS-CoV-2. Different vaccines have different advantages and limitations.
For example, whilst the mRNA vaccines may have higher efficacies and be easy to manufacture, the vector vaccines offer better opportunities to vaccinate in more isolated areas and less developed countries due to their easier storage requirements. mRNA vaccines require storage at very low temperatures due to the fragility of the mRNA.
Furthermore, the one-shot vaccines offer a more accessible approach and viral vectors may offer longer-term protection than mRNA vaccines.
There are four types of COVID-19 vaccines: here’s how they work
References
- Chung, Y. H., Beiss, V., Fiering, S. N. & Steinmetz, N. F. (2020) COVID-19 Vaccine Frontrunners and Their Nanotechnology Design. ACS Nano, 14(10). https://pubs.acs.org/doi/full/10.1021/acsnano.0c07197
- Department of Health and Social Care (DHSC) Pfizer Limited & BioNTech Manufacturing GmbH (2020) Public Assessment Report Authorisation for Temporary Supply COVID-19 mRNA Vaccine BNT162b2 (BNT162b2 RNA) concentrate for solution for injection. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/944544/COVID-19_mRNA_Vaccine_BNT162b2__UKPAR___PFIZER_BIONTECH__15Dec2020.pdf
- Li, Z. & Xu, X. (2019) Post-Translational Modifications of the Mini-Chromosome Maintenance Proteins in DNA Replication. Genes, 10(5). https://www.mdpi.com/2073-4425/10/5/331/htm
- The New York Times. 2021. Coronavirus Vaccine Tracker [online] Available at https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html [Accessed 18 March 2020]
- Voysey, M. et al. (2021) Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. The Lancet, 397(10269). https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32661-1/fulltex
Further Reading
Last Updated: Jan 17, 2022