The risk posed to researchers by this highly infectious agent – severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – currently dictates that live-virus research is performed under BSL3 conditions.
However, this requirement slows the speed of the response to this global pandemic, which continues to pose an unprecedented threat to public health and the worldwide economy.
Working with SARS-CoV-2 at a more accessible, lower biosafety level could expedite research. However, this requires the virus to be fully inactivated, without destroying the viral components needed for the research to be effective.

Researcher at US Centers for Disease Control, Atlanta, Georgia, working with influenza virus under biosafety level 3 conditions, with respirator inside a biosafety cabinet (BSC). Photo Credit: James Gathany Content Providers(s): CDC

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Now, Matthew Taylor and colleagues have validated and compared two protocols for SARS-CoV-2 inactivation – heat inactivation and ultraviolet (UV) irradiation – and described the effects that each technique had on virion components.
Both techniques effectively neutralized SARS-CoV-2, with each having different effects on important viral characteristics.
"We outline the strengths and weaknesses of each method so that investigators might choose the one which best meets their research goals," writes the team.
A pre-print version of the paper is available on the bioRxiv* server, while the article undergoes peer review.
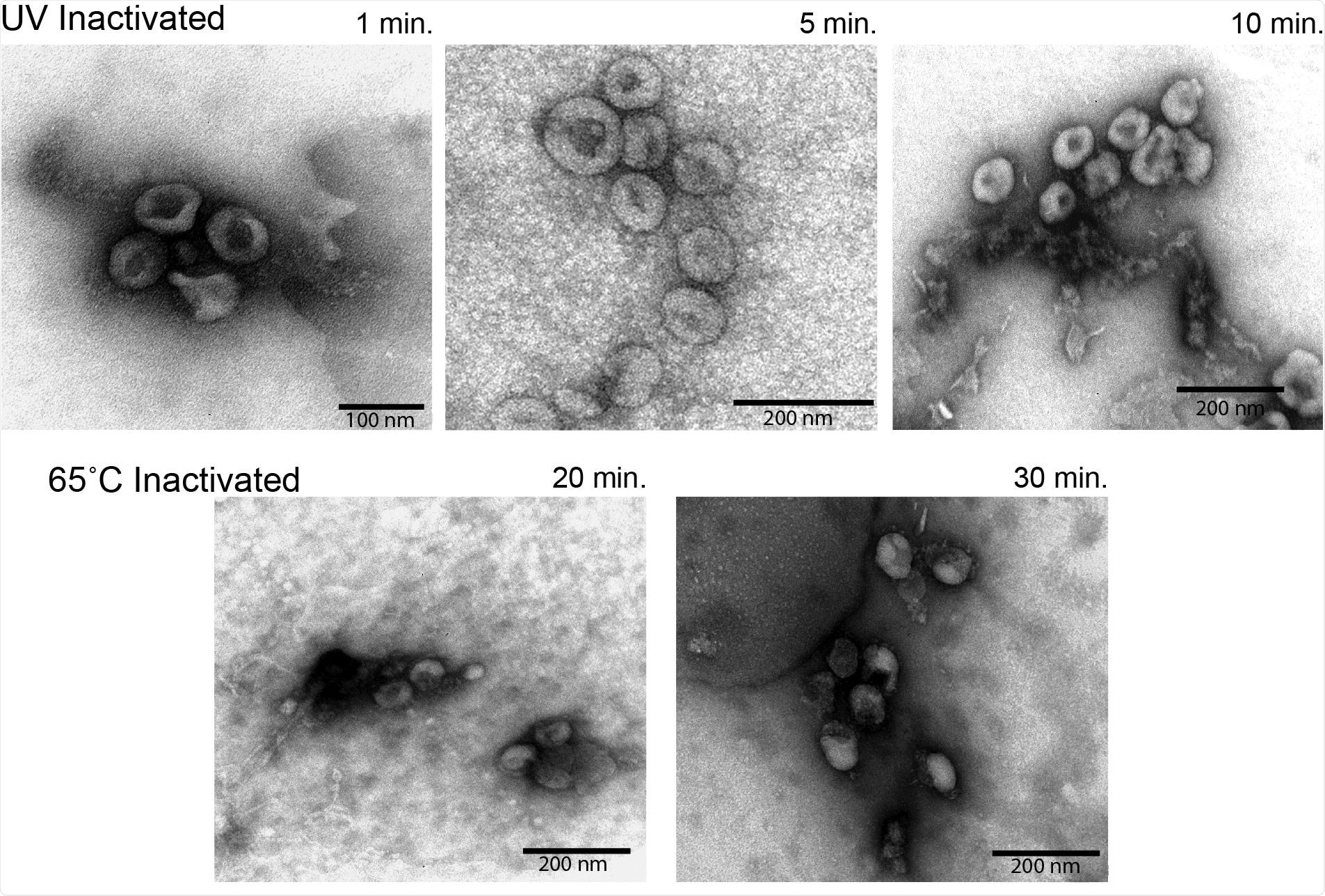
Electron microscopy analysis of virion morphology Semi-purified virion preparations were spotted onto a grid and imaged to assess virion morphology. The top row of images was taken from UV inactivated samples. The bottom row of images was taken from heat inactivated samples. Relative size is indicated by the scale bar in the lower corner of each image.
The challenges posed by BLS3 restrictions
Although confining SARS-CoV-2 research to BSL3 facilities only is highly effective at keeping researchers and the broader community safe, it limits the ability to provide the expedient response that is needed during this unprecedented pandemic.
"Viral inactivation can mitigate the risk of working with SARS-CoV-2 at a lower biosafety level, while expediting scientific objectives," write the researchers.
However, many of the SARS-CoV-2 inactivation methods that have been developed destroy the structural and genetic components that need to be kept intact for research to be effective.
"The most useful methods of inactivation are effective and reliable without being overly destructive to virion components," says the team.
What did the researchers do?
The team validated two SARS-CoV-2 neutralization techniques: heat inactivation and UV irradiation. Each method was optimized to ensure the virus was completely noninfectious and to limit any destructive effect on viral components.
For example, UV exposure was reduced by removing the plastic lids from Petri dishes that would otherwise absorb much of the incoming UV-C radiation, and heat inactivation was performed in low-volume tubes in a water bath to ensure that the heating and inactivation of samples was even throughout.
What did the study find?
Complete inactivation of high titer stocks of SARS-CoV-2 was achieved after just 15 minutes of incubation at 65˚C.
Complete inactivation was also achieved using one hundred times less UV power than has been used in comparable studies, says the team.
Although both techniques completely inactivated SARS-CoV-2, each method had unique effects on important viral characteristics that then affected downstream applications.
According to Taylor and colleagues, heat inactivation is ideal for preserving genetic material, while UV irradiation allows for the purification of high-quality virions.
The heat inactivation protocol left virions mostly intact, which the researchers say is an encouraging observation for protocols that enrich virions based on intact structures' biophysical properties. The heat treatment also left viral genomes mostly intact.
On the other hand, UV irradiation resulted in a 2-log reduction of detectable genomes, compared with heat inactivation.
"This made heat inactivation the preferred method for evaluations using genome-based assays like PCR," writes the team.
However, UV irradiation was especially effective at retaining virion morphology and antigenicity. High-resolution imaging of inactivated virions showed that UV-irradiated samples retained much of their native viral structure.
These samples were also significantly more detectable by enzyme-linked immunosorbent assay (ELISA), compared with the heat-treated samples.
The two inactivation protocols yielded near equivalent amounts of viral protein, although the quality of the proteins varied when assessed by Western blot. This is important to note if considering downstream applications for antigen detection or vaccine development, say the researchers.
Both methods are suitable for use in BSL2 environments
Taylor and colleagues say the findings show that both heat inactivation and UV irradiation represent viable SARS-CoV-2 inactivation methods for use in BSL2 facilities.
"Both methods left the virion mostly intact while effects on other viral properties differed," they write.
"From this study, it is clear that both the extent and method of inactivation have important ramifications on SARS-CoV-2 virions that should be considered when planning experiments or downstream applications," concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Taylor M, et al. Effects of inactivation method on SARS-CoV-2 virion proteins and structure. medRxiv, 2020. doi: https://doi.org/10.1101/2020.11.14.383026, https://www.biorxiv.org/content/10.1101/2020.11.14.383026v1
- Peer reviewed and published scientific report.
Loveday, Emma K., Kyle S. Hain, Irina Kochetkova, Jodi F. Hedges, Amanda Robison, Deann T. Snyder, Susan K. Brumfield, et al. 2021. “Effect of Inactivation Methods on SARS-CoV-2 Virion Protein and Structure.” Viruses 13 (4): 562. https://doi.org/10.3390/v13040562. https://www.mdpi.com/1999-4915/13/4/562.