Very common – most of us will experience bowel symptoms from time to time, but usually the symptoms last only a few days. You should see your GP if they persist for more than three weeks (sooner if they are severe) or if your symptoms keep coming back.
© Sebastian Kaulitzki / Shutterstock.com
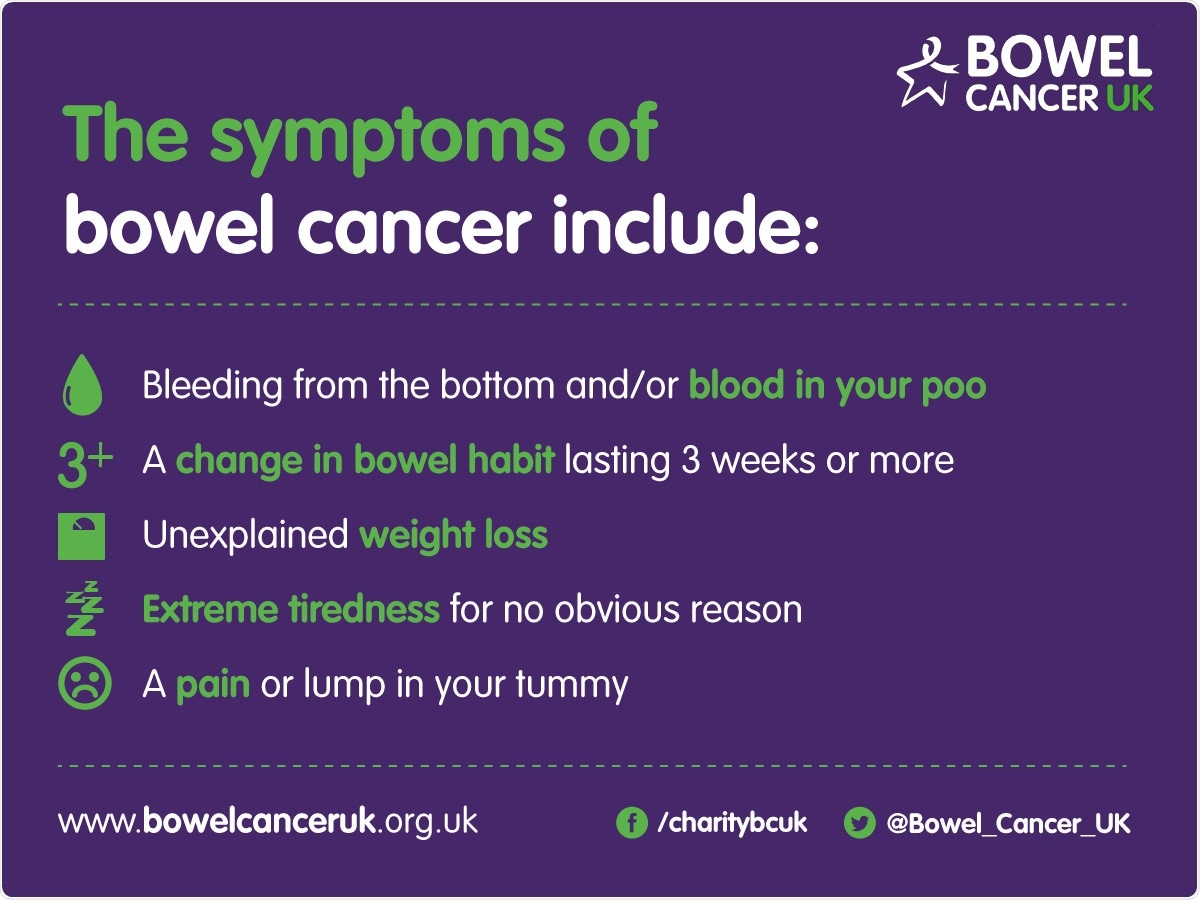
The key signs you could have bowel cancer include:
- bleeding from your bottom, and/or blood in your poo
- a change in bowel habit lasting three weeks or longer
- unexplained weight loss
- extreme tiredness for no obvious reason
- a pain or lump in your tummy
Most of the time, a person suffering these symptoms won’t have bowel cancer or inflammatory bowel disease, but it is better to be sure.
What are the different causes of lower bowel symptoms?
Most bowel symptoms are caused by harmless disorders such as piles, irritable bowel syndrome (a “sensitive bowel”) or a short-lived bowel infection (gastroenteritis).
However there are a range of more serious conditions such as inflammatory bowel disease, coeliac disease or bowel cancer – the earlier they are diagnosed the more effectively they can be treated.
How do GPs distinguish between serious and non-serious bowel conditions?
This can be difficult because of the common nature of bowel symptoms, the wide range of potential bowel complaints and the significant overlap of symptoms between complaints.
It can be particularly difficult to identify significant disease in young people, where it is less common. This was the main reason why we did our research – to identify which symptoms and findings are most predictive of identifying either bowel cancer or inflammatory bowel disease in younger people.
Are there any particular symptoms associated with a high probability of colorectal cancer (CRC) or inflammatory bowel disease (IBD)?
Our study identified ten features that were independently associated with bowel cancer or inflammatory bowel disease.
The most predictive were for rectal bleeding in combination with diarrhoea or certain blood test findings ( thrombocytosis, low MCV, low haemoglobin or raised inflammatory markers), for change in bowel habit with certain blood test findings (low MCV, thrombocytosis or low haemoglobin) and for diarrhoea with the blood test finding of thrombocytosis.
Therefore in terms of patient symptoms, the key ones are change in bowel habit or diarrhoea and rectal bleeding.
How many people does CRC and IBD affect?
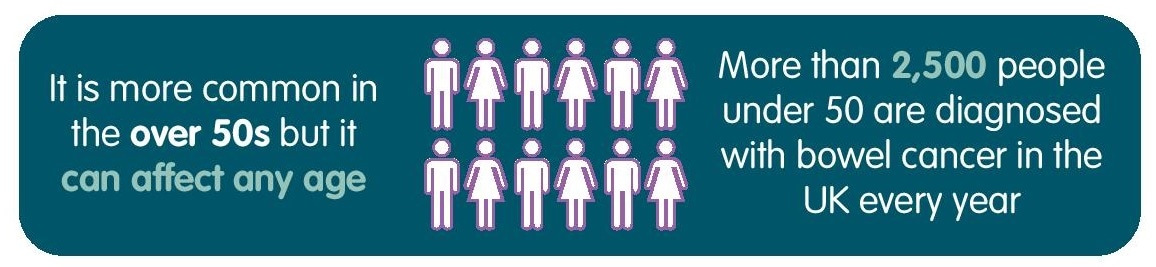
About 1 in 20 of us will develop bowel cancer during our lifetime. About 41,000 people are diagnosed with bowel cancer in the UK every year – including over 2,500 under-50s.
It is estimated that there are about 260,000 people living with IBD in the UK – it affects about 1 in 250 of us. Across all ages 13,000 people are diagnosed with inflammatory bowel disease each year, of which many are under 50.
Can these conditions affect young people?
IBD is often diagnosed in people in their late teens or early 20s, but can affect people of any age.
Whilst bowel cancer predominantly affects people over the age of 60, a significant minority may develop the disease at a younger age – so yes, it can affect young people too.
Can you please outline the new risk assessment tool funded by the Department of Health to support GPs to identify the symptoms of a serious bowel condition for patients aged under-50?
The University of Exeter, in partnership with our Never Too Young campaign, Durham University and North Tees and Hartlepool NHS Foundation Trust have published new research and a risk assessment tool to support GPs to identify the symptoms of a serious bowel condition for patients aged under-50.
The bowel cancer and inflammatory bowel disease risk assessment tool, published in the British Journal of General Practice and funded by the Department of Health, aims to support GPs to determine which patients need further tests by predicting the level of risk depending on the patient’s symptoms. Using symptoms, a physical examination and blood test results, the tool calculates the risk of a serious disease with a percentage, as well as suggesting next steps.
How was this tool developed?
The bowel cancer and inflammatory bowel disease risk assessment tool, published in the British Journal of General Practice and funded by the Department of Health, is a matched case-control study using primary care records from the Clinical Practice Research Datalink, UK.
Incident cases (aged <50 years) of bowel cancer and IBD diagnosed between 2000 and 2013 were each matched with up to three controls. Odds ratios and positive predictive values were estimated for features of bowel cancer and IBD in the year before diagnosis.
What impact do you think this tool will have?
We hope that the tool will help GPs to identify young patients most at risk of either IBD or bowel cancer, referring them for hospital tests at an earlier stage.
Where can readers find more information?
More information about the study is available on Bowel Cancer UK’s website, which also contains a wealth of other information about the disease.
For IBD, Crohn’s and Colitis UK have an excellent website.
Information is also available from the NHS Choices website.
About Professor Matt Rutter MBBS MD FRCP (London, Edinburgh)
 Matt Rutter is Professor of Gastroenterology at Durham University and the University Hospital of North Tees. He specialises in advanced diagnostic colonoscopy, polypectomy and IBD. He sits on the BSG Endoscopy Research committee and the governing board of ESGE. He chairs the ESGE Quality Improvement in Endoscopy committee and the BCSP Research Advisory Committee.
Matt Rutter is Professor of Gastroenterology at Durham University and the University Hospital of North Tees. He specialises in advanced diagnostic colonoscopy, polypectomy and IBD. He sits on the BSG Endoscopy Research committee and the governing board of ESGE. He chairs the ESGE Quality Improvement in Endoscopy committee and the BCSP Research Advisory Committee.
He has published and lectured worldwide on quality in endoscopy, screening and colonoscopic surveillance, receiving the BSG Hopkins Endoscopy Prize in 2006 and the RCP Goulstonian Lectureship in 2008. He co-authored BSG (2010), NICE (2011), European (ECCO, 2012) and SCENIC (USA, 2015) colitis surveillance guidelines, and was the lead author for the BSG/ACPGBI management of large non-pedunculated colorectal polyps guidelines (2015).
He is regional screening lead for QA in colonoscopy, GI research lead for North East & North Cumbria LCRN and is one of the core faculty for the Northern Region Endoscopy Training Centre.