The association of SARS-CoV-2 infection (NeuroCOVID) with damage to the nervous system is not clearly understood. The non-exclusive mechanisms that can lead to NeuroCOVID can include invasion of the brain by the virus along the cranial nerve pathways or disruption of the blood barrier (BBB) and compartmentalized or deleterious systemic immune response within the central nervous system (CNS). Understanding these mechanisms is vital for developing therapeutic targets and strategies for preventing long-term neurological impact in NeuroCOVID patients.
 Study: Cerebrospinal fluid biomarkers in SARS-CoV-2 patients with acute neurological syndromes. Image Credit: Kateryna Kon / Shutterstock
Study: Cerebrospinal fluid biomarkers in SARS-CoV-2 patients with acute neurological syndromes. Image Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
NeuroCOVID might increase the risk of developing a neurodegenerative disorder or might speed up its progression. Several factors can trigger a neurodegenerative cascade in NeuroCOVID patients, including the vulnerability of some brain areas to SARS-CoV-2 infection and dysregulation of genes important for neuronal survival by SARS-CoV-2, as well as gut microbiota dysregulation by SARS-CoV-2 infection and its impact on the brain. Other factors that lead to depression, extended stay in the intensive care unit (ICU), severe sepsis, or post-traumatic stress could also be associated with the risk of cognitive decline post-SARS-CoV-2 infection.
Most of the previous studies on consequences of SARS-CoV-2 infection on CNS highlighted neurodegeneration, acute neuronal injury, or neuroinflammation while only a few focused on biomarkers that characterized these different mechanisms. Therefore, further studies are required comprising large, well-characterized NeuroCOVID patients to understand the CNS damage pathogenesis and prevent it.
A new research paper, under review in the Molecular Neurobiology journal and currently available on the Research Square* preprint server, studied several biomarkers associated with neuronal injury, neuroinflammation, and neurodegeneration in NeuroCOVID adults who experienced a CNS syndrome during acute SARS-CoV-2 infection.
About the study
The study involved 24 COVID-19 confirmed patients who experienced neurological symptoms between March 2020 and June 2021. Confirmation of SARS-CoV-2 infection was undertaken using real-time protein chain reaction (RT-PCR).
Data on the patients' medical history, along with neurophysiological recordings and clinical, neuroradiological, and biological investigations, were collected during their hospital stay. Patients were classified as having meningoencephalitis or encephalopathy and the disease severity was defined as moderate, mild, severe, or critical.
The plasma and cerebrospinal fluid (CSF) were screened to detect any co-infections. Finally, CSF biomarkers for neurodegeneration and neuronal injury and CSF neopterin for neuroinflammation, were quantified.
Study findings
The results reported that the median age of the patients was 62 years, no patient had a history of neurological disease, and most of the patients were male. Encephalopathy was reported to be the primary neurological syndrome, although eight patients developed movement disorders and five experienced strokes. The disease severity was observed to be either moderate, severe, or critical, and hospitalized patients in the ICU were found to benefit from mechanical ventilation.
The patients reported a lumbar puncture within 5 days of neurological symptom onset. Only CSF pleocytosis, albumin ratio, and protein levels were found to be elevated in meningoencephalitis patients, while no other difference in biomarkers was observed. Isoelectric focusing patterns 2 and 3 were observed in 50% of patients with severe disease, 25% of patients with moderate disease, and 70% of those with critical disease. Moreover, the level of CSF neopterin was found to be increased in 75% of the patients.
The CSF neurofilament light chain (NfL) levels were found to be higher in patients, while no correlation was found with age, duration of ICU stay, and lumbar puncture. The total tau protein levels were also found to be increased and a positive correlation between NfL CSF and T-tau levels was also observed.
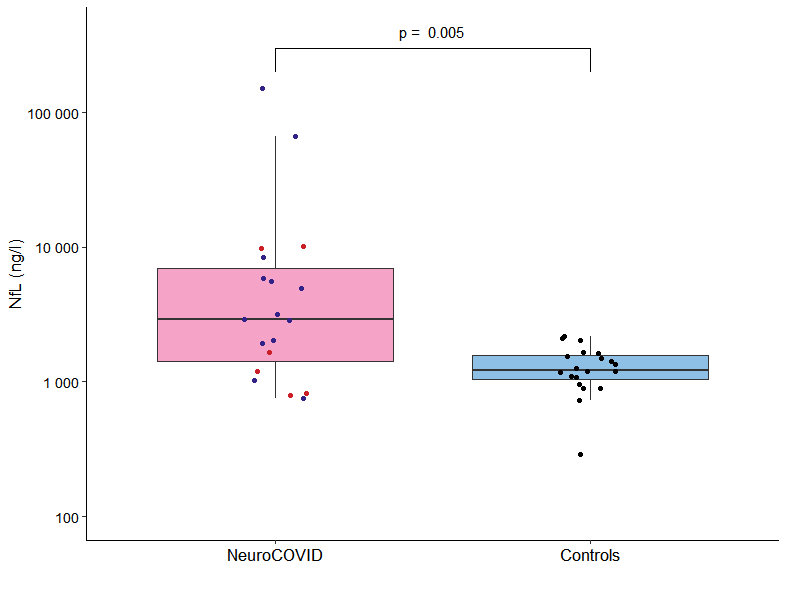
Level of CSF NfL in NeuroCOVID group and controls Boxplots of cerebrospinal fluid (CSF) neurofilament light chain (NfL) in NeuroCOVID (n=19, 13 encephalopathies in blue and six meningoencephalitis in red) and controls of non-COVID patients with psychiatric illnesses (n=20, in black)
The Aß1-42 peptide was found to be low in 11 patients out of which two had meningoencephalitis and nine had encephalopathy. The CSF NfL concentration was also found to be increased in these patients; however, the tau protein levels were found to be normal. No patient had a typical CSF pattern indicative of Alzheimer's disease.
Therefore, the current study demonstrated the elevation of CSF biomarkers of neuronal injury and neuroinflammation in severe NeuroCOVID patients. This could lead to neuronal damage and disruption of amyloid precursor peptide processing. Thus, anti-inflammatory drugs are essential during the early stages of the disease. Further studies are required to confirm whether SARS-CoV-2-induced neuronal injury could lead to a chronic neurodegenerative process.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources