Modern treatments for heart failure (HF) patients with low ejection fraction (EF), which indicates systolic function impairments in the cardiovascular system, may improve EF. However, data on managing HF patients with improved ejection fraction (HFimpEF), a condition usually excluded from HF outcome assessment trials, are limited.
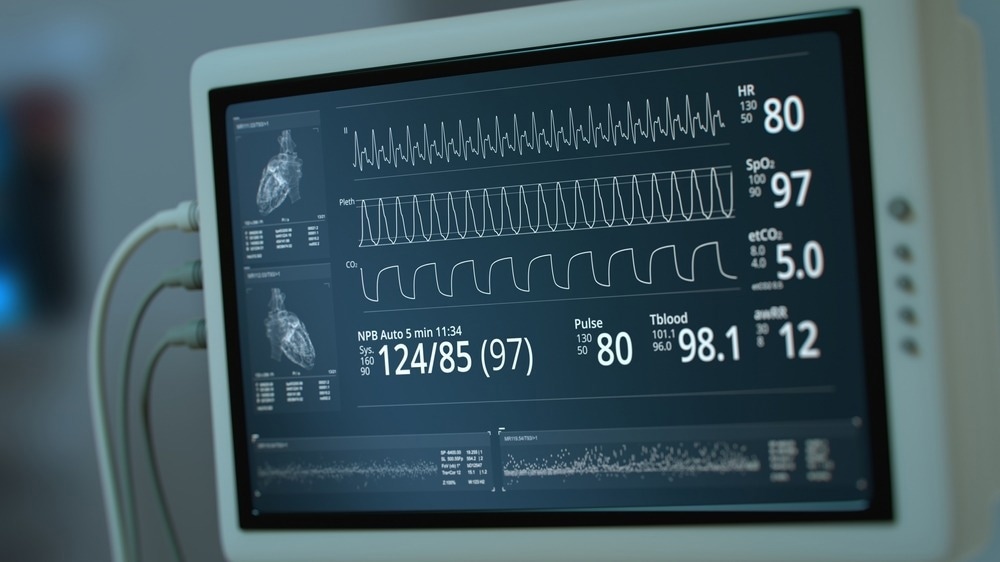
Study: Dapagliflozin in heart failure with improved ejection fraction: a prespecified analysis of the DELIVER trial. Image Credit: SquareMotion / Shutterstock.com
About the study
The DELIVER trial is a prospective, international, double-blinded, randomized, placebo-controlled clinical trial conducted across 353 locations from 20 nations to evaluate the safety and efficacy of dapagliflozin compared to placebo among HF patients with mildly lowered preserved or increased EF.
Among 6,263 DELIVER trial participants with symptomatic HF and left ventricular EF of more than 40%, 18% of individuals had HFimpEF, with EF increasing from less than or equal to 40% to more than 40%.
Between September 1, 2018, and January 18, 2021, 3,131 and 3,132 individuals were allocated to receive 10 mg of dapagliflozin or placebo, respectively, daily, stratified by diabetes mellitus type 2 status. The study comprised individuals aged 40 years or older with LVEF greater than 40% within one year of enrolment and symptomatic HF.
Furthermore, all study participants exhibited elevated natriuretic peptide levels (NT-proBNP), defined as NT-proBNP exceeding 300 pg/ml among individuals with no atrial fibrillation/flutter or over 600 pg/ml among those with atrial fibrillation/flutter. Structural cardiac illness was also present in all study participants, including left ventricular hypertrophy or left atrial enlargement.
Individuals with/without diabetes mellitus type 2 and those hospitalized or provided care in outpatient settings for worsening heart failure were included in the study. In addition, individuals with a prior history of LVEF values equal to or less than 40% but greater than 40.0% echocardiogram (ECG) values during enrolment were also included.
The team excluded individuals who used sodium/glucose cotransporter 2 (SGLT2) inhibitors within four weeks of treatment allocation, prior SGLT2 inhibitor intolerance, diabetes mellitus type 1, systolic blood pressure reading exceeding 160 mm of Hg, and not taking more than three antihypertensive drugs, estimated glomerular filtration rate (EGFR) values less than 25 ml/min/1.7 m2, as well as those who had systolic blood pressure exceeding 180 mm of Hg, irrespective of the antihypertensive drugs prescribed.
In addition, individuals with diagnoses accountable for HF symptoms, including primary pulmonary hypertension and anemia, were excluded from the analysis.
The prime study outcome was a composite measure of deteriorating HF or death from cardiovascular disease. Secondary study outcomes included the total number of HF events, such as initial and subsequent hospital admissions for HF or urgent HF visits, cardiovascular deaths, the Kansas-city cardiomyopathy questionnaire (KCCQ) score-assessed quality of life, cardiovascular disease-related mortality, and all-cause deaths.
HFimpEF patients were identified based on their answers to a question investigating the history of symptomatic HF with lowered EF of less than or equal to 40%. Follow-up assessments were performed after one, four, eight, 12, and 16 months post-randomization and every four months after that.
Cox proportional-hazards modeling was used to evaluate the prime and secondary outcome data. Hazard ratios (HR) were also calculated. Semi-parametric Cox modeling was performed to analyze cardiovascular deaths and total HF events.
Study findings
HFimpEF patients had comparable event rates as individuals with EF less than 40%. Among HFimpEF patients, dapagliflozin lowered the prime composite study outcome with an HR of 0.7, first worsening HF events with an HR of 0.8, cardiovascular deaths with an HR of 0.6, and total worsening HF events to comparable levels among individuals with EF greater than 40%.
Among HFimpEF patients, the advantage of dapagliflozin as compared to the placebo was consistently observed across the pre-specified LVEF subgroups, with HR values of 0.8, 0.7, and 0.6 for LVEF values less than or equal to 49%, 50% to 59%, and greater than 60.0%, respectively.
Rates of cardiovascular deaths, first HF events, all-cause deaths, and total HF events were comparable among HFimpEF patients and individuals with LVEF greater than 40%. However, out of 3,131 individuals, 18% had a history of prior LVEF of less than or equal to 40%.
Compared to individuals with LVEF exceeding 40%, HFimpEF patients were younger, more likely to be male, less likely to be White, and had lower LVEF baseline values.
A more significant proportion of HFimpEF patients than individuals with LVEF greater than 40% had a history of coronary artery disease and myocardial infarctions. These individuals were also more likely to have been previously hospitalized due to HF or had implantable cardioverter defibrillators (ICDs).
HFimpEF patients, in comparison to individuals with LVEF exceeding 40%, were more likely to be treated at baseline with angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, mineralocorticoid receptor antagonists, or angiotensin receptor neprilysin inhibitors. These results were consistent after adjusting for sex, geographical region, and age.
Dapagliflozin-treated participants improved their KCCQ scores more than those who received the placebo, regardless of HFimpEF status. Analyzing KCCQ data from one, four, and eight months showed similar findings.
Serious adverse events resulting in dapagliflozin discontinuation were observed among 18 HFimpEF patients, ten of whom received dapagliflozin and eight placebo-treated individuals. Serious adverse events also occurred among 56 individuals with LVEF exceeding 40%, 32 of whom were treated with dapagliflozin and 24 placebo-treated individuals.
Overall, the study findings indicate that symptomatic HFimpEF patients might benefit from dapagliflozin treatment to reduce their morbidity and death risk.
Journal reference:
- Vardeny, O., Fang, J.C., Desai, A.S. et al. (2022). Dapagliflozin in heart failure with improved ejection fraction: a prespecified analysis of the DELIVER trial. Nature Medicine. doi:10.1038/s41591-022-02102-9