In a study published in the journal Nature Metabolism, researchers treated male mice on a high-fat diet (HFD) with an inhibitor of mitochondrial transcription (IMT). They found that this shifted the mice's metabolism towards fatty acid oxidation, leading to weight loss, reversal of hepatosteatosis, and improved glucose tolerance. Further, they observed reduced oxidative phosphorylation (OXPHOS) capacity and upregulation of fatty acid oxidation in the liver, indicating a rewiring of mitochondrial metabolism caused by reduced mitochondrial deoxyribonucleic acid (mtDNA) expression.
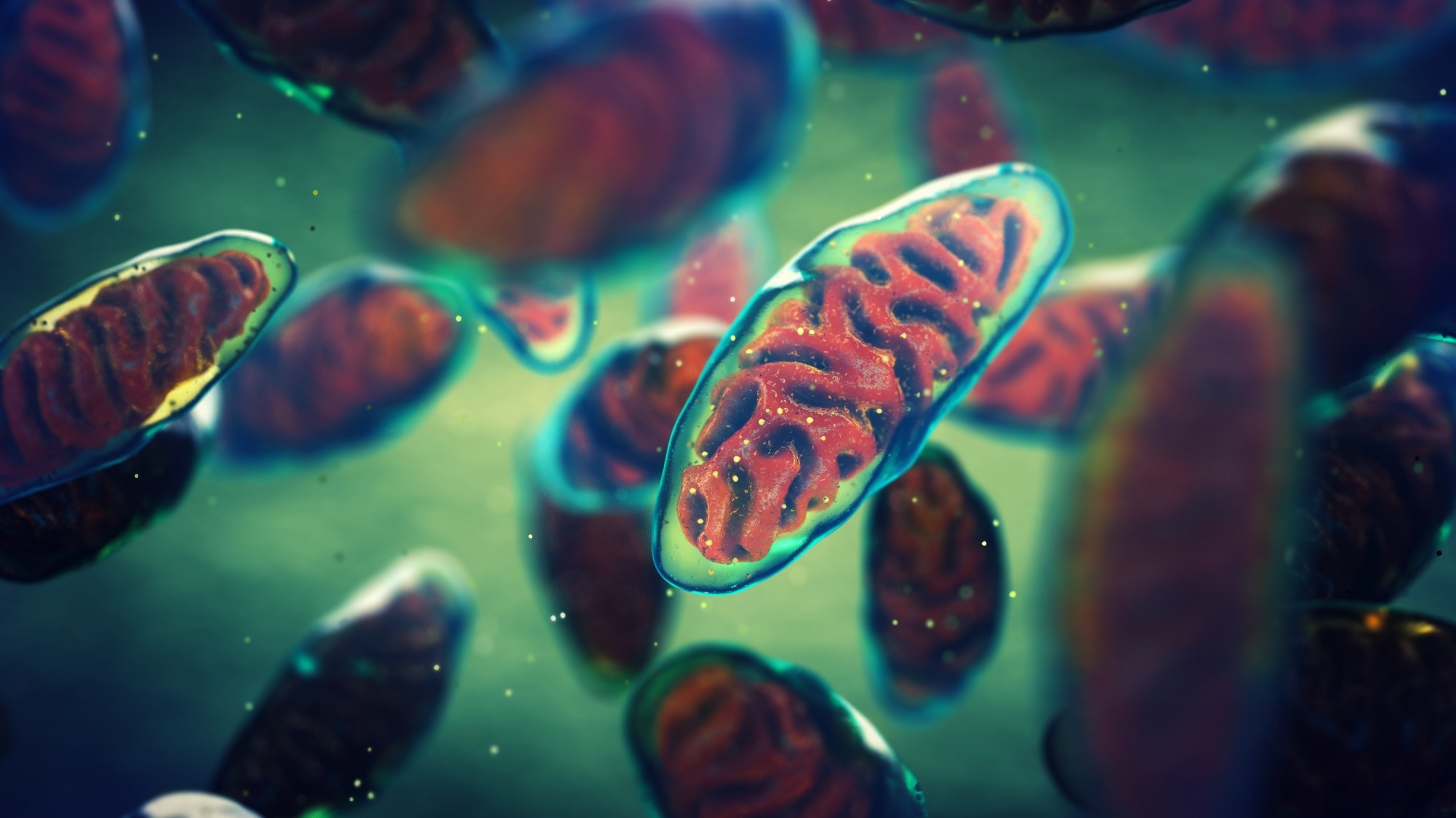 Study: Inhibition of mammalian mtDNA transcription acts paradoxically to reverse diet-induced hepatosteatosis and obesity. Image Credit: nobeastsofierce / Shutterstock
Study: Inhibition of mammalian mtDNA transcription acts paradoxically to reverse diet-induced hepatosteatosis and obesity. Image Credit: nobeastsofierce / Shutterstock
Background
In the 1930s, attempts to target mitochondria for obesity treatment with dinitrophenol (DNP) showed promise but were hindered by serious side effects. Metformin, a mild complex I inhibitor used to inhibit OXPHOS, is effective against diabetes and cancer. Given the potential link between metabolic benefits and anti-cancer properties of mitochondrial-targeting drugs, researchers investigated whether the inhibitor of mitochondrial transcription (IMT), known to impede tumor metabolism, could yield beneficial metabolic effects. IMT treatment in tumor cell lines disrupted OXPHOS, leading to metabolic starvation and cell death. Despite drastic effects on cancer cells, IMT treatment in whole animals was well-tolerated. Therefore, researchers in the present study aimed to investigate whether administering IMT to animals, with the goal of moderately reducing their OXPHOS capacity, could lead to positive metabolic effects in both healthy and metabolically challenged mice.
About the study
Male C57BL/6N mice were divided into chow or HFD groups for eight weeks, then subdivided for 4-week treatment with IMT or vehicle. Mice were monitored using the Comprehensive Lab Animal Monitoring System (CLAMS) for five days. Fecal lipid content, energy content, and respiratory exchange ratio (RER) were analyzed. Blood glucose and serum insulin levels were measured, and intraperitoneal glucose tolerance tests (ipGTT) were conducted. Glucose-stimulated insulin secretion (GSIS) assays were performed using isolated pancreatic islets.
Liver histology was assessed to examine hepatosteatosis, and lipid content in the liver was measured. Lipidomics analysis was performed to assess lipid profiles, while serum aminotransferase activities and albumin levels were measured to evaluate liver function. Label-free quantitative proteomics was used to identify differentially expressed proteins in liver tissue and mitochondria.
Results and discussion
"Four weeks of treatment led to an unexpected increase in fat metabolism, resulting in a drastic weight loss, a reduction in fat accumulation in the liver, and restored glucose tolerance." – Taolin Yuan (Postdoctoral Researcher)
IMT treatment in HFD-fed mice rapidly reduced body weight by approximately 7 g after four weeks, primarily due to decreased fat mass without affecting lean mass. Histological analysis showed reduced adipocyte size in white adipose tissue. IMT treatment did not affect food intake, physical activity, or fecal lipid content. There was no significant change in total energy content in feces, suggesting IMT-induced weight loss is not due to malabsorption.
IMT treatment increased oxygen consumption in mice on HFD, suggesting enhanced metabolism. However, the analysis did not clearly link this effect to increased energy expenditure. Instead, IMT treatment lowered the RER, indicating enhanced fat metabolism. These findings suggest that IMT reverses high-fat diet-induced obesity by promoting fat metabolism at the organismal level.
HFD-fed mice exhibited normal fasting blood glucose but elevated fasting serum insulin, indicative of insulin resistance. IMT treatment improved glucose homeostasis by reducing fasting blood glucose and serum insulin levels and normalizing ipGTT responses. IMT lowered circulating insulin without affecting insulin secretion or biosynthesis in isolated pancreatic islets. Enhanced glucose homeostasis in IMT-treated HFD-fed mice likely resulted from increased insulin sensitivity.
IMT treatment significantly reduced hepatosteatosis in HFD-fed mice, accompanied by decreased liver lipid content and weight. A reversal of diglyceride and triglyceride accumulation was observed in the liver. Liver function improved with reduced serum aminotransferase activities. Serum albumin levels remained normal. These results indicate that IMT effectively reversed diet-induced hepatosteatosis and normalized liver function.
IMT treatment significantly reduced mtDNA-encoded transcripts and mtDNA levels in mouse liver, likely due to impaired ribonucleic acid (RNA) primer formation essential for mtDNA replication. It moderately decreased mtDNA levels in epididymal white adipose tissue (eWAT) but had no significant impact on skeletal muscle, heart, or brown adipose tissue (BAT). IMT concentrations were significantly higher in the plasma and liver compared to other tissues, indicating preferential accumulation in the liver. This skewed tissue distribution explains the pronounced inhibitory effect of IMT on mtDNA transcription in the liver.
IMT treatment significantly altered approximately 15–20% of the 4,408 proteins identified in the liver tissue proteome, majorly mitochondrial proteins. IMT treatment significantly altered OXPHOS subunit levels and respiratory chain enzyme activities, particularly reducing complex I, I/III, and IV activities while maintaining complex II and II/III activities. IMT was found to rewire liver metabolism to aid fatty acid degradation, leading to potential obesity reversal.
Conclusion
"It's exciting that we have identified a new potential strategy for treating common diseases like obesity and type 2 diabetes." – Professor Nils-Göran Larsson (Principal Investigator).
In conclusion, the study provides strong evidence that IMT treatment enhances fatty acid oxidation in the liver of mice fed HFD. The metabolic changes resulting from decreased mtDNA expression in the liver offer a potential strategy for drug therapy targeting obesity and associated pathologies. Further research using isotope-labeled substrates in isolated liver cells or whole animals is warranted to confirm these findings.